Revitalising the NHS: A Comprehensive Blueprint for Sustainable Healthcare
Artificial IntelligenceRevitalising the NHS: A Comprehensive Blueprint for Sustainable Healthcare
:warning: WARNING: This content was generated using Generative AI. While efforts have been made to ensure accuracy and coherence, readers should approach the material with critical thinking and verify important information from authoritative sources.
Table of Contents
- Revitalising the NHS: A Comprehensive Blueprint for Sustainable Healthcare
- Introduction: The NHS at a Crossroads
- Harnessing Data and Digital Technologies
- Optimizing the NHS Workforce
- Reimagining Patient-Centered Care
- Sustainable Funding and Resource Allocation
- Fostering Cross-Sector Collaboration
- Conclusion: A Roadmap for NHS Transformation
Introduction: The NHS at a Crossroads
Historical Context and Current Challenges
The NHS's Founding Principles and Evolution
The National Health Service (NHS) stands as a cornerstone of British society, embodying the nation's commitment to universal healthcare. Since its inception in 1948, the NHS has been guided by a set of founding principles that have shaped its evolution and continue to influence its operation today. Understanding these principles and the NHS's journey through the decades is crucial for appreciating the current challenges it faces and the imperative for transformation.
- Comprehensive care: Meeting the needs of everyone
- Free at the point of delivery: Based on clinical need, not ability to pay
- Equality of access: Available to all citizens
- Funded through central taxation: A collective responsibility
These founding principles represented a radical departure from previous healthcare models, establishing a system that aimed to provide equitable access to medical care for all citizens, regardless of their socioeconomic status. The NHS quickly became a source of national pride and a model for healthcare systems worldwide.
Over the decades, the NHS has undergone significant evolution in response to changing demographics, medical advancements, and societal expectations. Key milestones in its development include the introduction of prescription charges in 1952, the reorganisation of services in the 1970s, and the implementation of internal markets in the 1990s. Each of these changes sought to address emerging challenges while maintaining the core principles of the service.
The NHS has been the envy of the world for decades, but it must continue to evolve to meet the changing needs of our population and the advances in medical science.
The turn of the millennium brought new challenges and opportunities. The advent of digital technologies, the rising costs of advanced treatments, and an ageing population have all placed increasing pressure on the NHS. The service has responded with initiatives such as the NHS Plan in 2000, which aimed to increase investment and reform service delivery, and the Health and Social Care Act of 2012, which introduced significant structural changes to the organisation of healthcare in England.
Despite these efforts, the NHS today faces unprecedented challenges. Waiting times for treatments have reached record highs, staff shortages are chronic across many specialties, and the integration of health and social care remains a complex issue. The COVID-19 pandemic has further exposed and exacerbated these systemic weaknesses, while simultaneously demonstrating the NHS's capacity for rapid innovation and adaptation under pressure.
- Increasing demand due to an ageing population
- Rising costs of medical technologies and treatments
- Workforce shortages and retention issues
- Integration challenges between health and social care
- Inequalities in health outcomes across different communities
As we look to the future, the NHS stands at a critical juncture. The challenge lies in preserving its founding principles while adapting to the realities of 21st-century healthcare. This requires a delicate balance between tradition and innovation, between universal access and financial sustainability, and between centralised coordination and local responsiveness.
We must honour the vision of the NHS's founders while embracing the transformative potential of new technologies and care models to ensure its sustainability for future generations.
The evolution of the NHS reflects the changing face of British society and the ever-advancing field of medicine. Its journey from a post-war vision to a modern, complex health system offers valuable lessons for its future development. As we consider how to address the current challenges facing the NHS, we must draw upon this rich history, learning from both its successes and its setbacks to chart a course towards a more resilient and effective healthcare system for all.
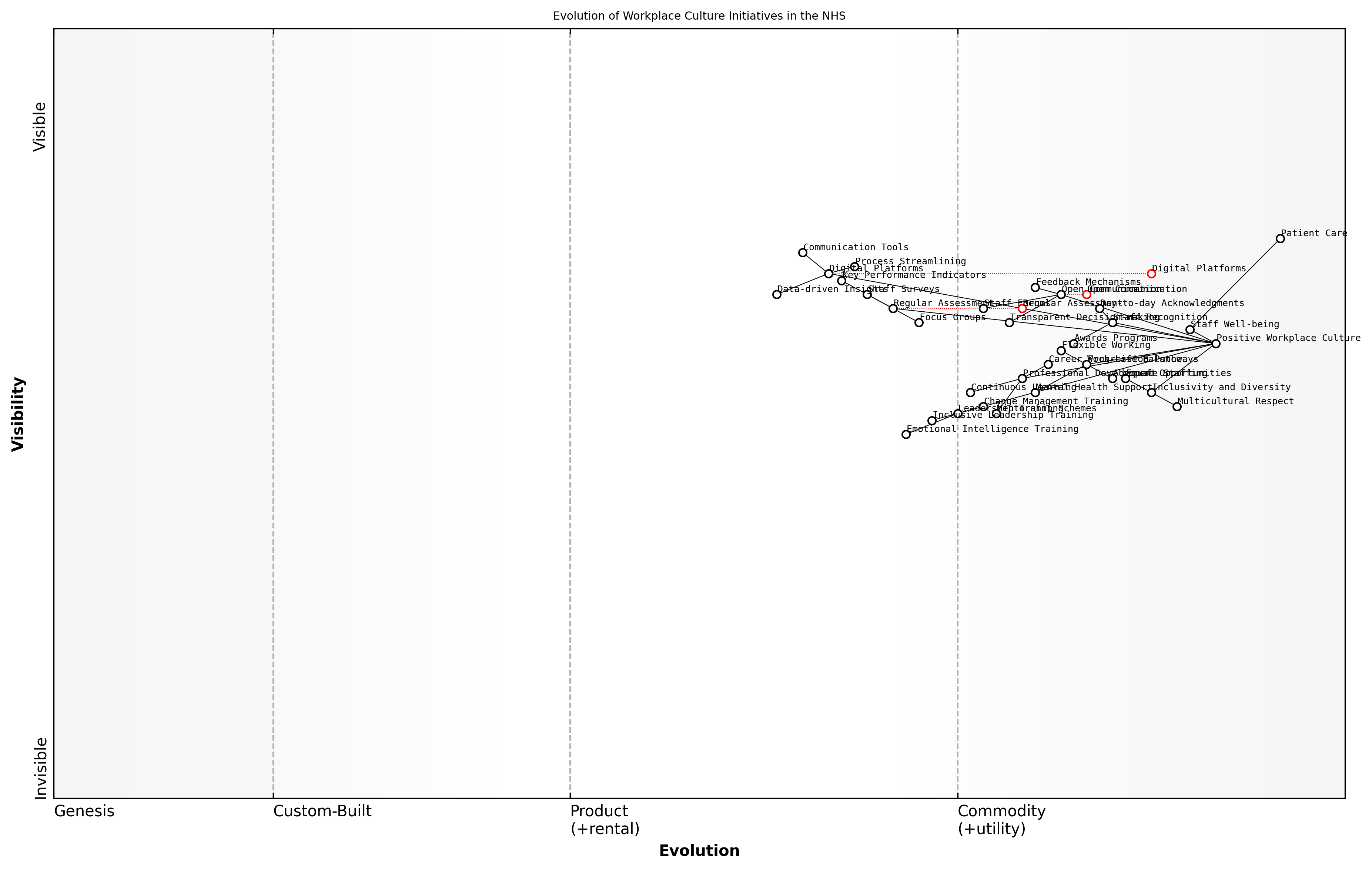
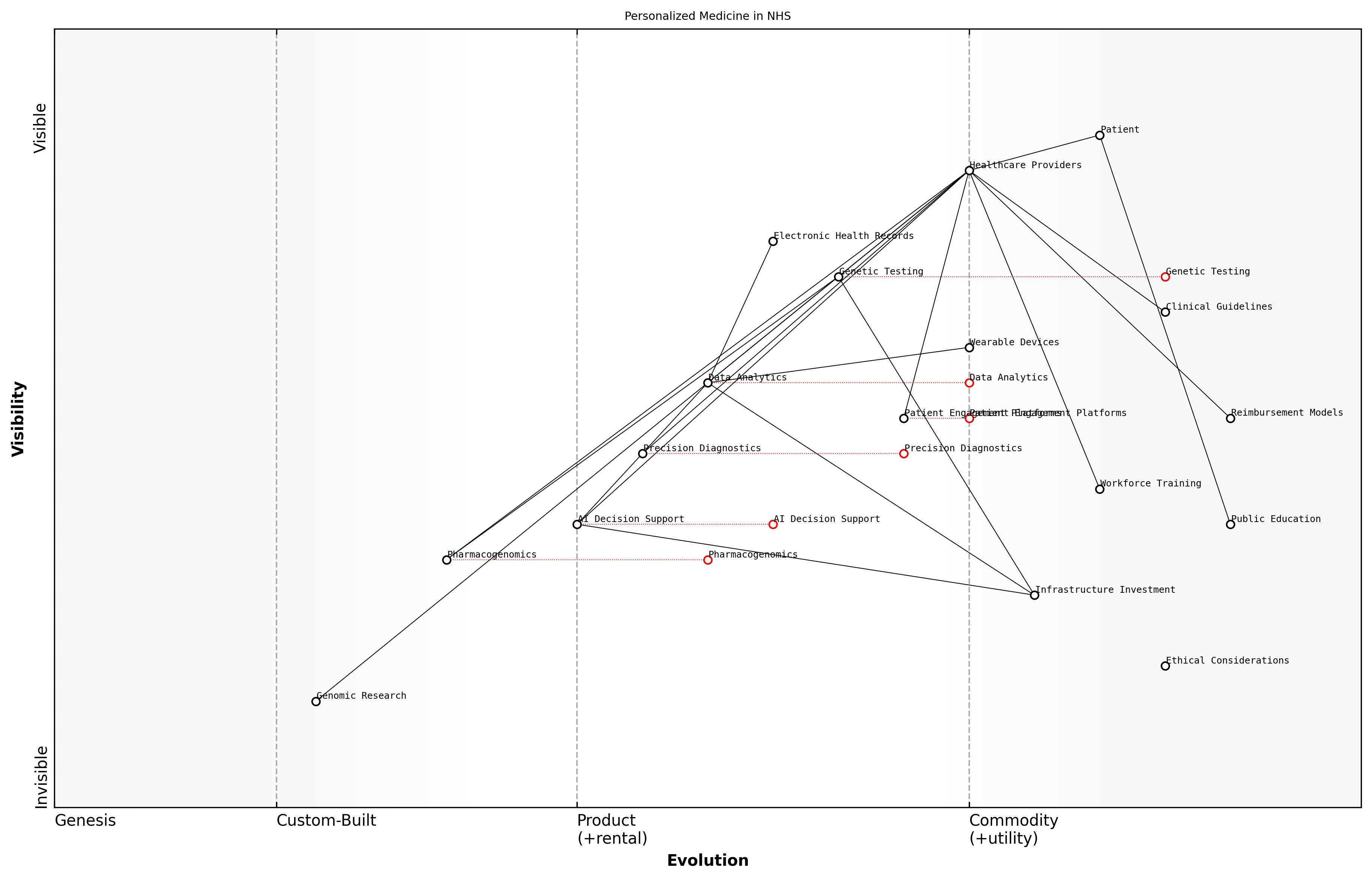
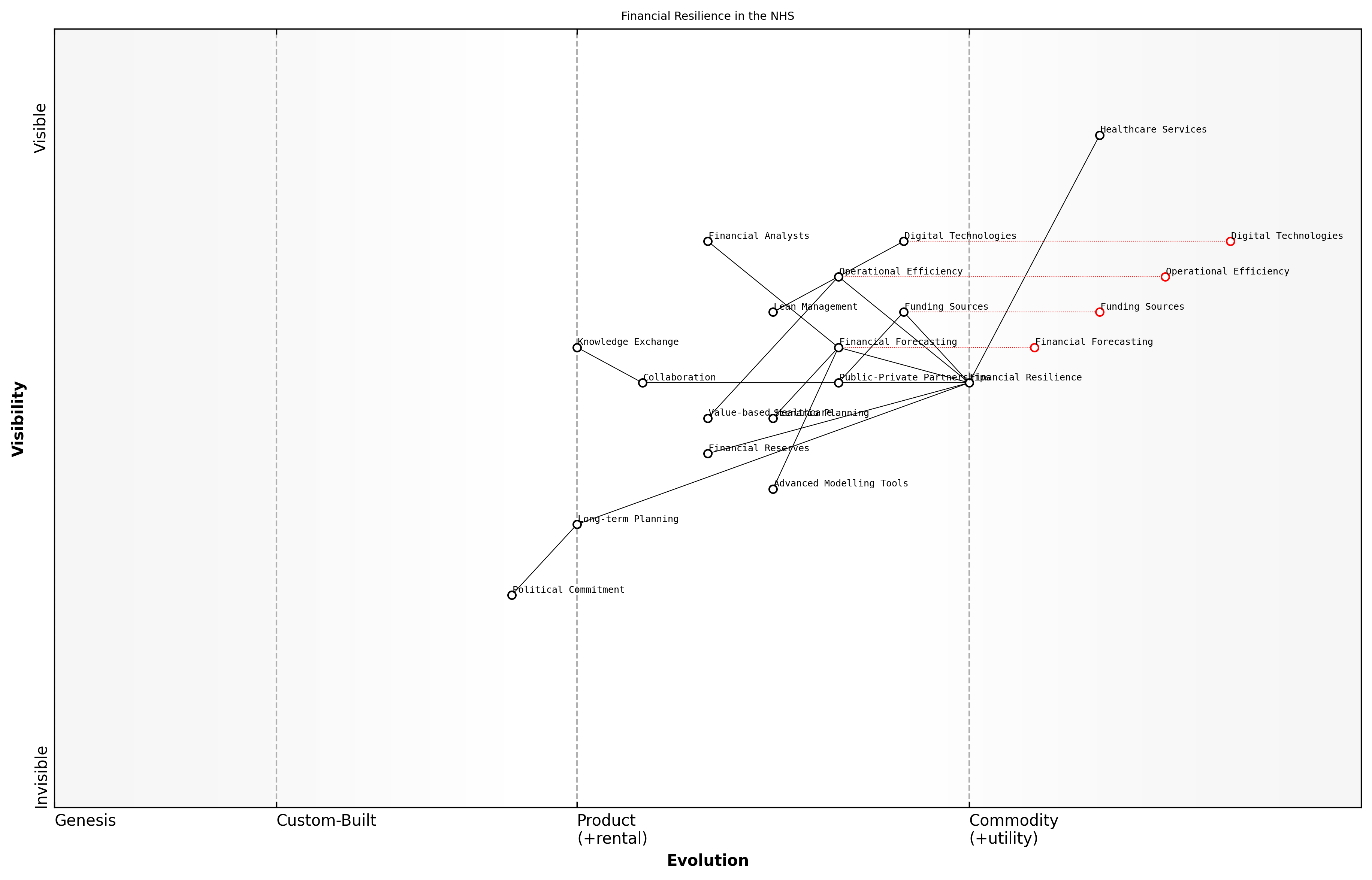
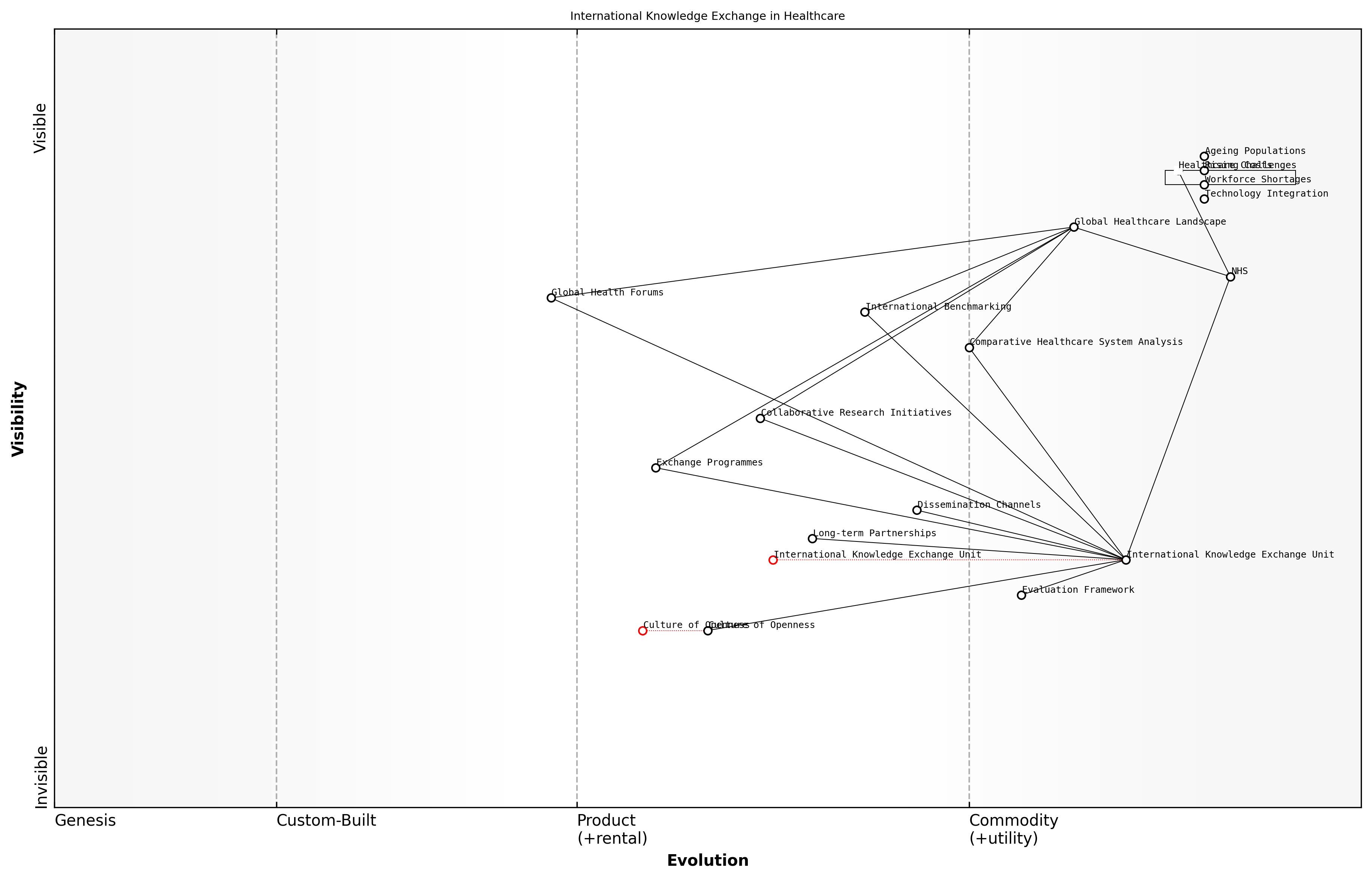
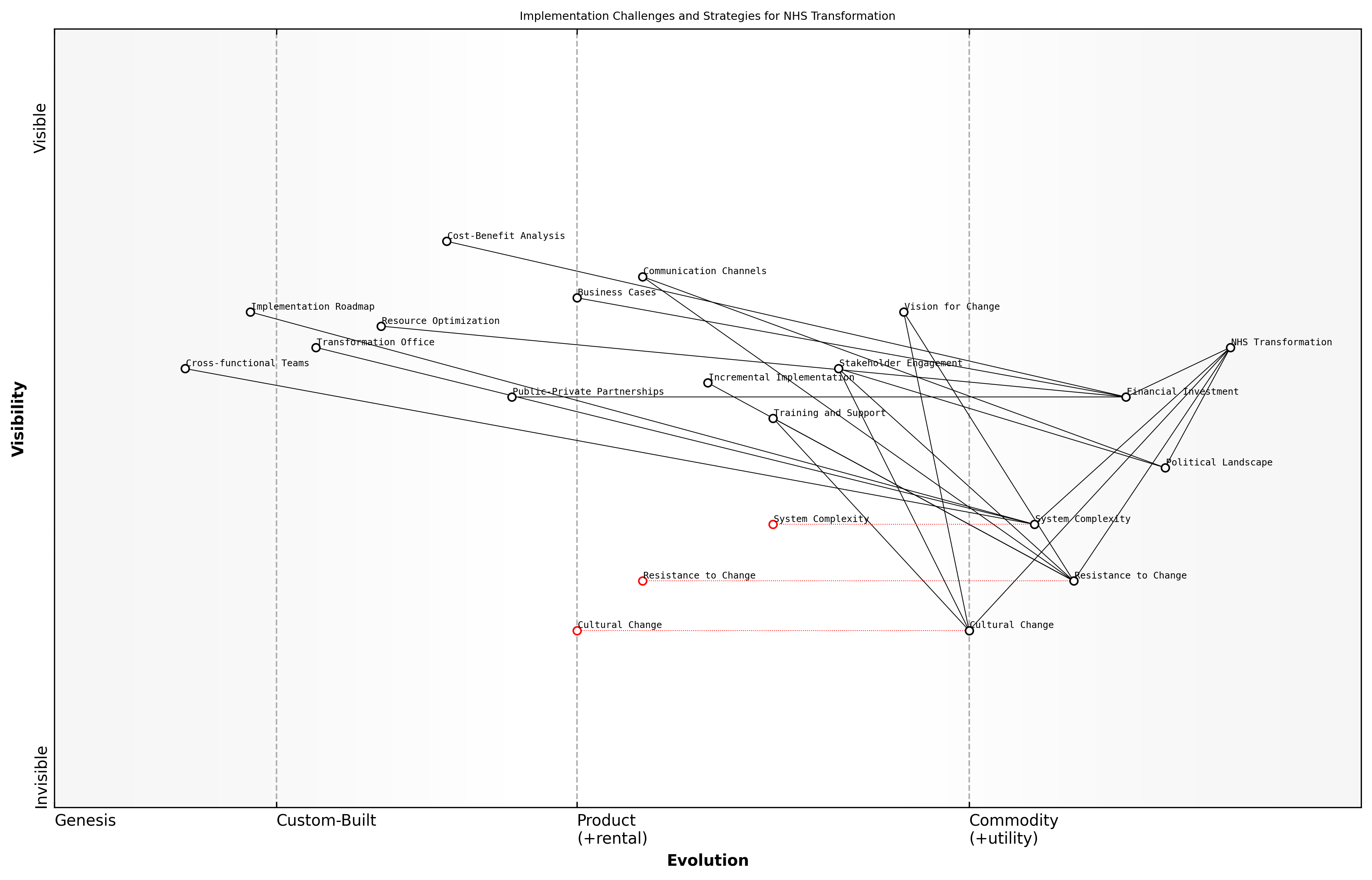
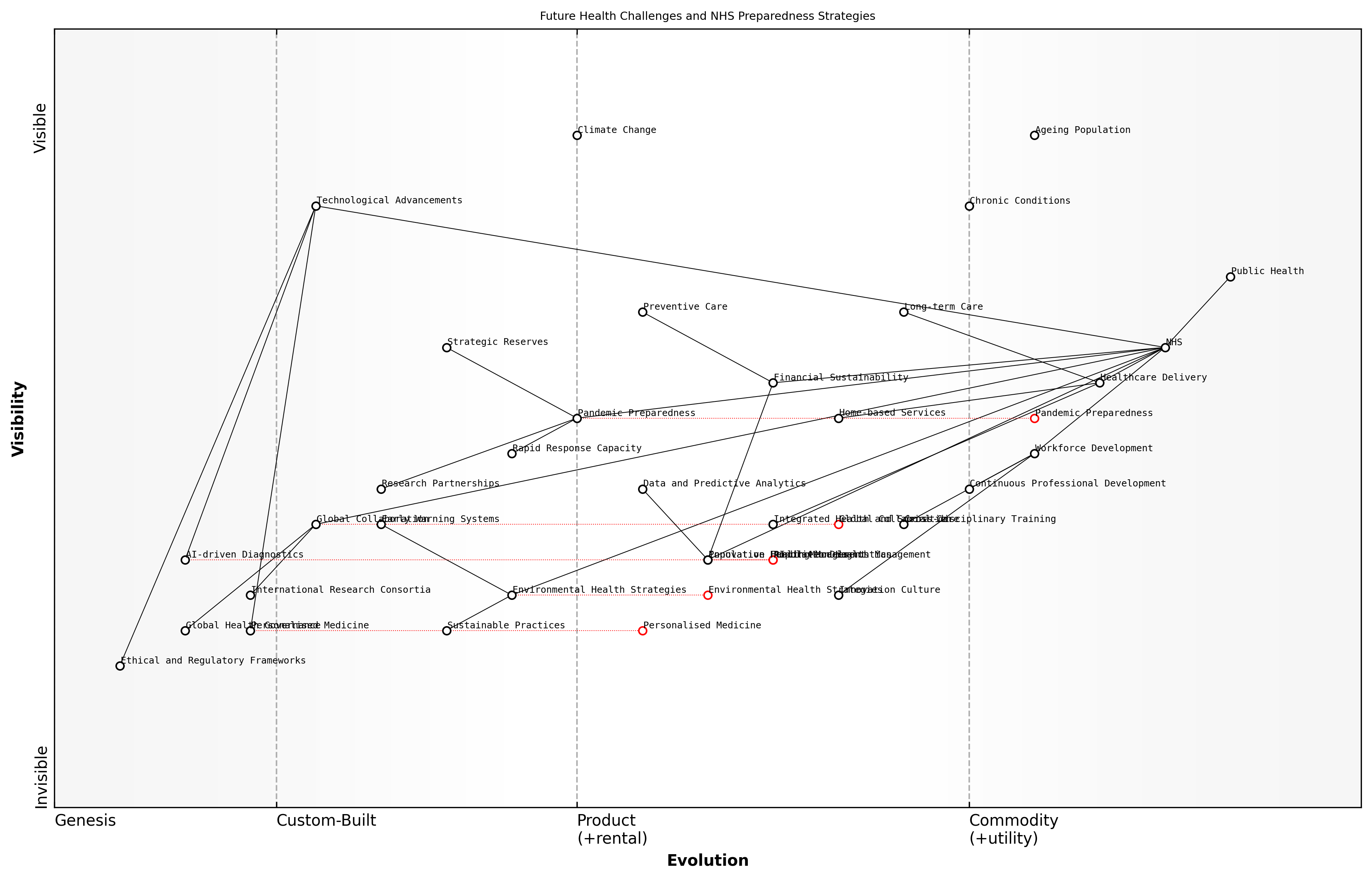
Wardley Map Assessment
The NHS is at a critical juncture, facing challenges from an ageing population and increasing demand, while also having opportunities to leverage digital technologies and innovative care models. The strategic focus should be on maintaining the core founding principles while rapidly evolving healthcare delivery through digital transformation, workforce development, and ecosystem integration. Success will require balancing short-term operational improvements with long-term structural changes, all while ensuring that innovations align with the NHS's fundamental mission of providing comprehensive, free, and equitable healthcare.
[View full Wardley Map report](markdown/wardley_map_reports/wardley_map_report_01_english_The NHS's Founding Principles and Evolution.md)
Present-day Pressures and Systemic Issues
The National Health Service (NHS) in the United Kingdom is currently facing an unprecedented array of challenges that threaten its ability to deliver high-quality, universal healthcare. These pressures and systemic issues are the result of a complex interplay of demographic shifts, technological advancements, economic constraints, and evolving societal expectations. As we delve into these challenges, it becomes clear that the NHS is at a critical juncture, requiring innovative solutions and systemic reforms to ensure its sustainability and effectiveness in the 21st century.
- Ageing population and increasing chronic disease burden
- Workforce shortages and retention issues
- Technological advancements and the need for digital transformation
- Rising costs and funding constraints
- Increasing demand for services and longer waiting times
- Health inequalities and disparities in access to care
- Integration challenges between health and social care
- Mental health service pressures
- Impact of Brexit on healthcare workforce and research
- COVID-19 pandemic aftermath and service backlogs
One of the most significant pressures facing the NHS is the ageing population and the associated increase in chronic diseases. The UK's demographic shift towards an older population has led to a surge in complex, long-term health conditions that require ongoing management and care. This trend has placed immense strain on NHS resources, both in terms of hospital capacity and community-based services. The challenge is not merely about providing more care, but about fundamentally restructuring services to meet the changing needs of the population.
The NHS is grappling with a perfect storm of increased demand, workforce shortages, and financial constraints. We need to radically rethink how we deliver care to meet the needs of an ageing population with multiple chronic conditions.
Workforce issues represent another critical pressure point for the NHS. The service is facing severe shortages across various healthcare professions, including nurses, doctors, and allied health professionals. These shortages are exacerbated by high turnover rates, burnout, and challenges in recruitment and retention. The situation has been further complicated by Brexit, which has impacted the NHS's ability to recruit from EU countries. Addressing these workforce challenges is crucial for maintaining service quality and meeting growing demand.
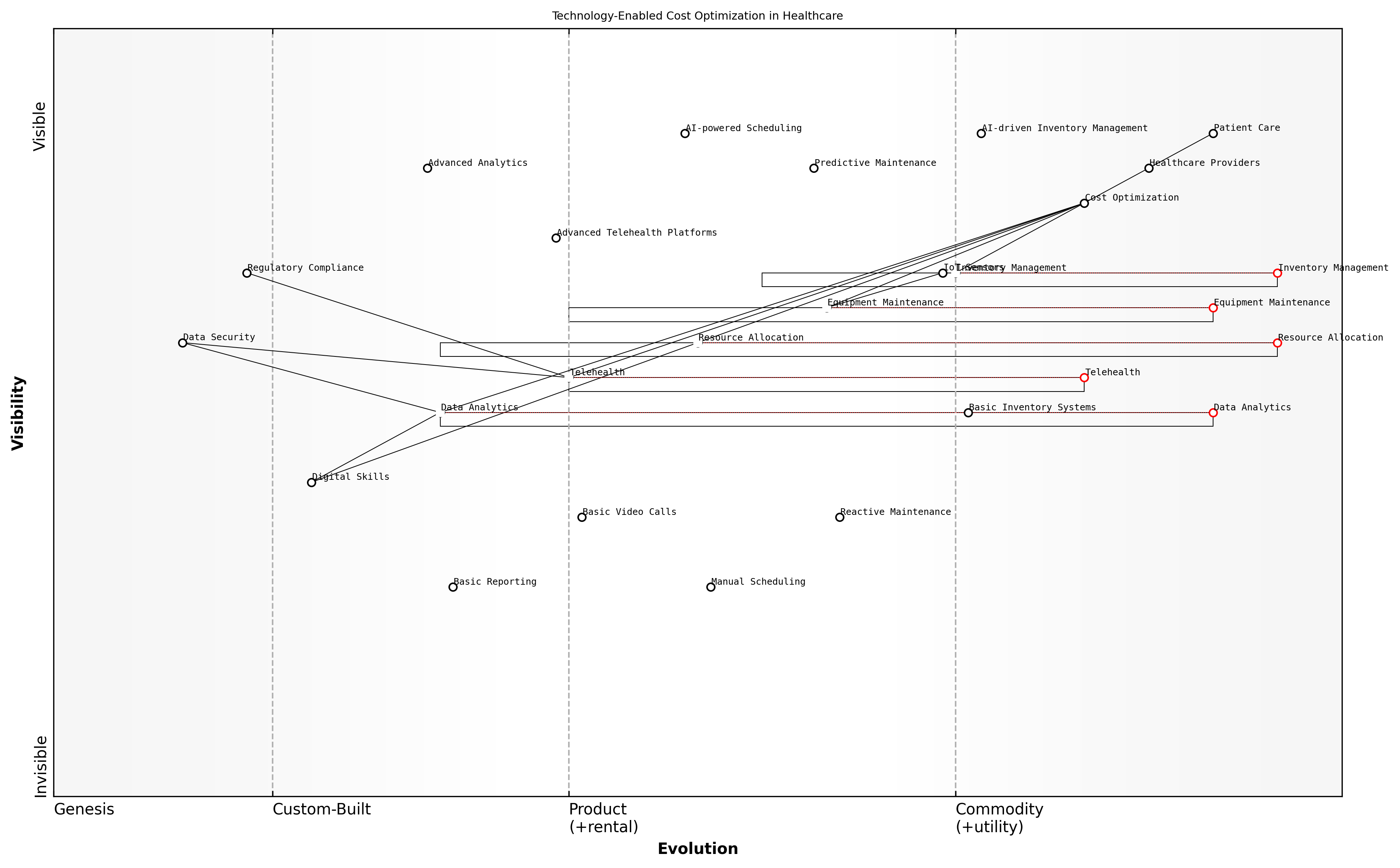
The rapid pace of technological advancement presents both opportunities and challenges for the NHS. While innovations in medical technology, artificial intelligence, and digital health solutions offer the potential to improve care quality and efficiency, they also require significant investment and organisational change. The NHS has struggled to keep pace with digital transformation, leading to inefficiencies, data silos, and missed opportunities for improving patient care and operational effectiveness.
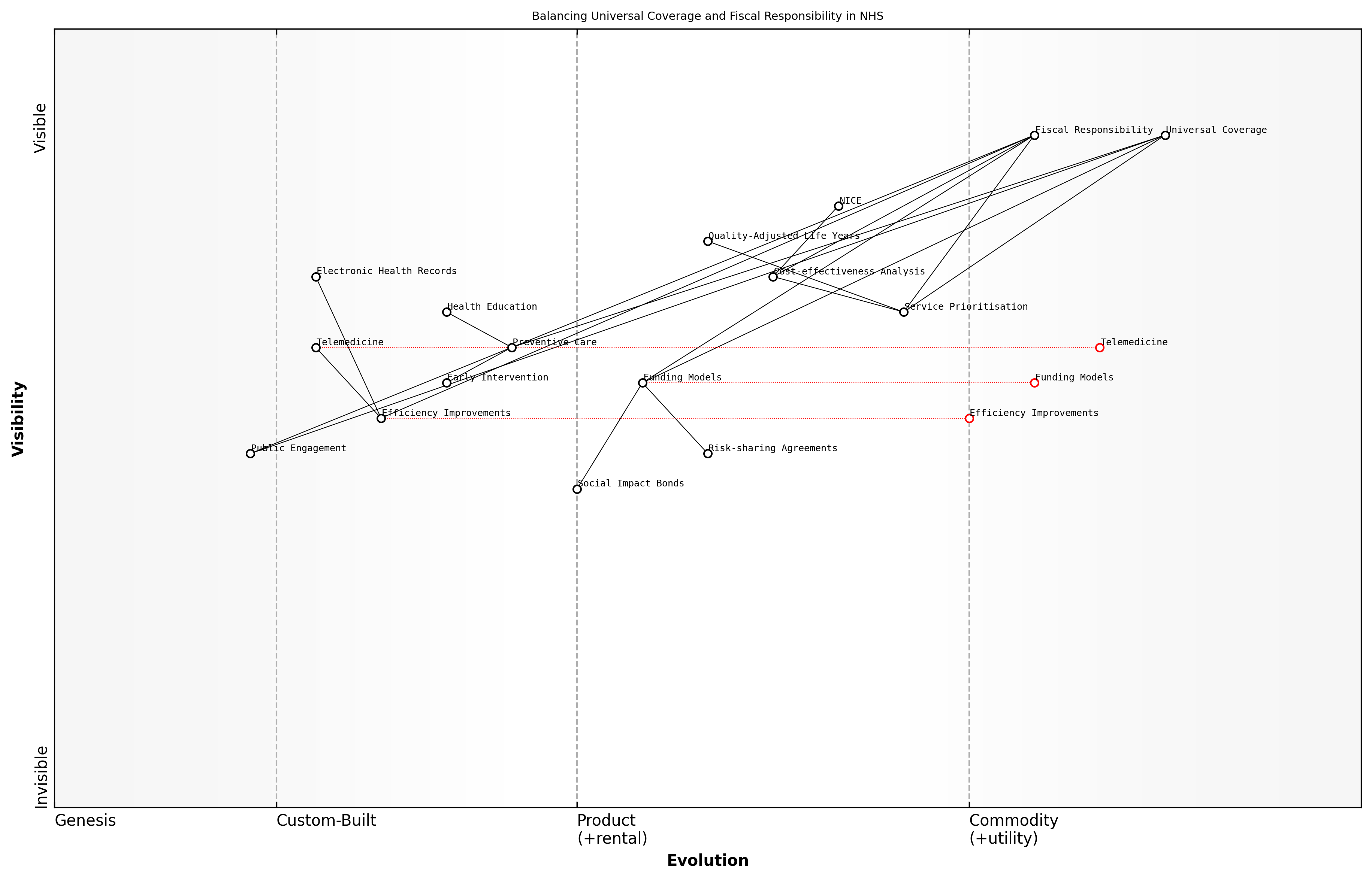
Financial pressures continue to be a major systemic issue for the NHS. Despite increases in funding, the service faces a significant gap between available resources and the cost of meeting growing demand. This financial strain is compounded by rising costs of new treatments and technologies, as well as the need to address long-standing infrastructure issues. The challenge of balancing fiscal responsibility with the commitment to universal healthcare coverage remains a central tension in NHS policy and planning.
The financial sustainability of the NHS is not just about more money; it's about fundamentally rethinking how we allocate resources, incentivise efficiency, and measure value in healthcare delivery.
Increasing demand for services, coupled with capacity constraints, has led to longer waiting times across many areas of NHS care. This issue has been dramatically exacerbated by the COVID-19 pandemic, which has created significant backlogs in elective procedures and routine care. Addressing these waiting lists while simultaneously managing ongoing acute care needs represents a major challenge for the NHS in the coming years.
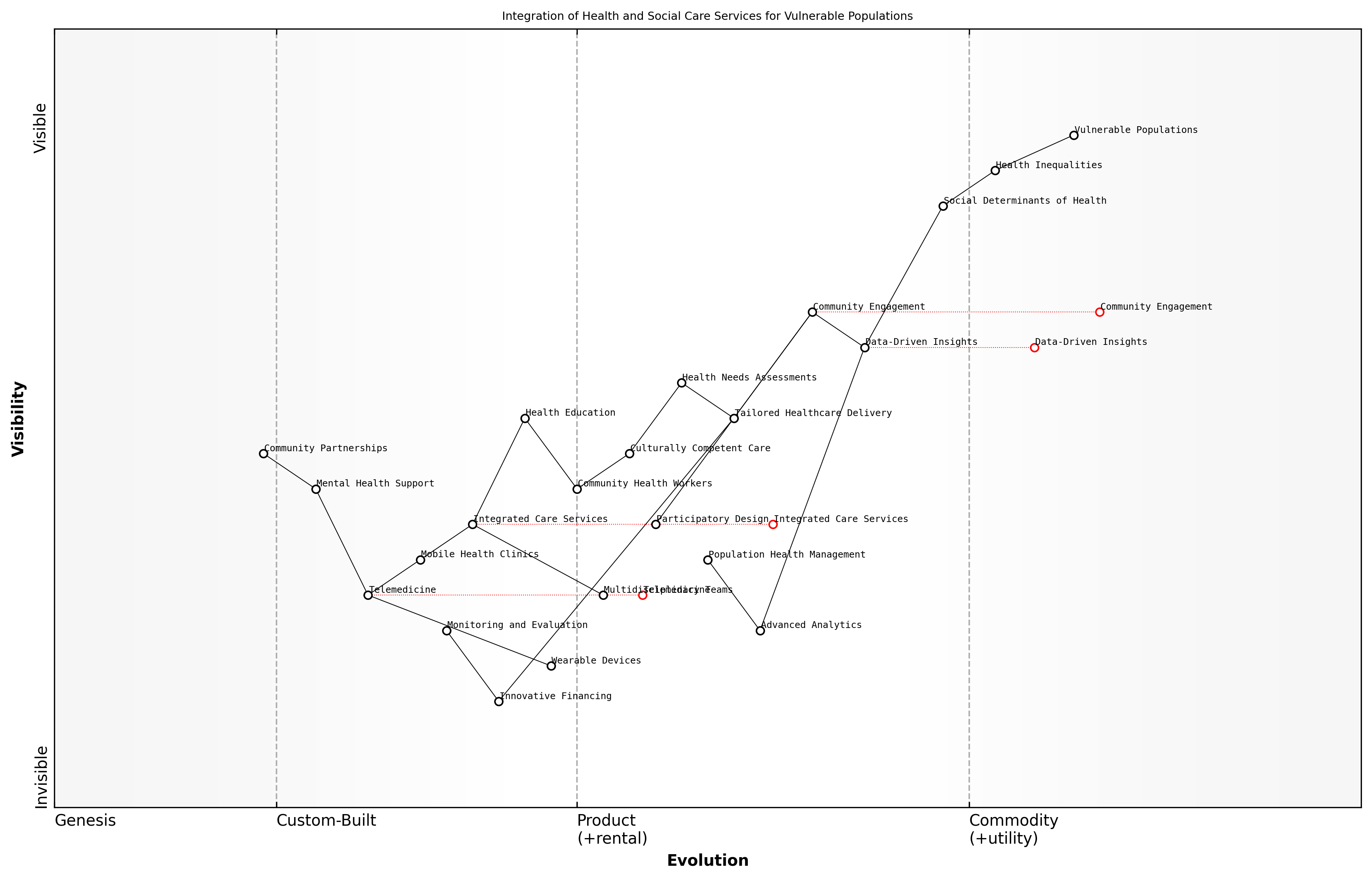
Health inequalities remain a persistent and troubling issue within the NHS. Despite the service's founding principle of equitable access to healthcare, significant disparities exist in health outcomes and access to services based on factors such as socioeconomic status, ethnicity, and geographic location. Addressing these inequalities requires not only targeted healthcare interventions but also broader action on the social determinants of health.
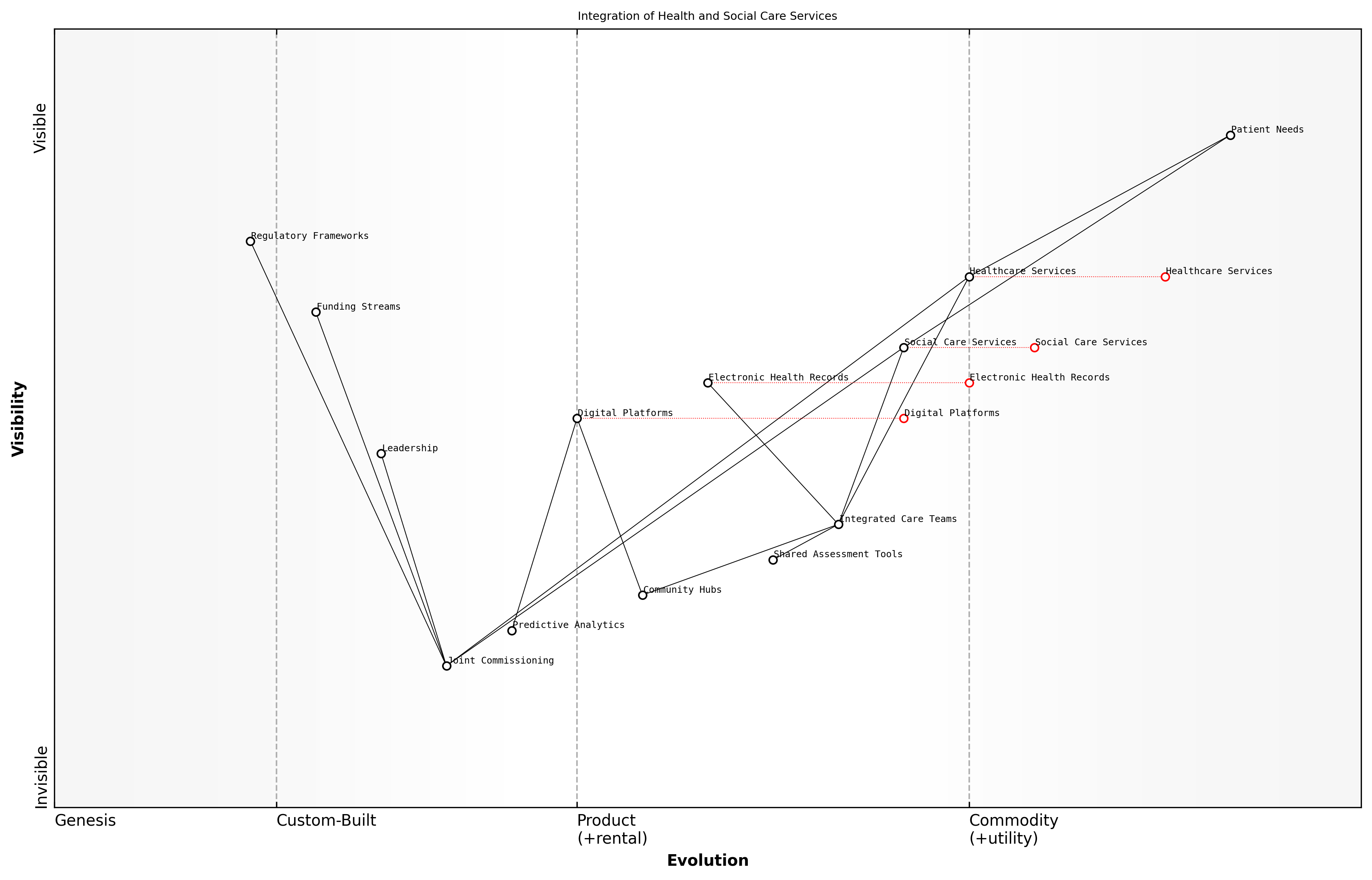
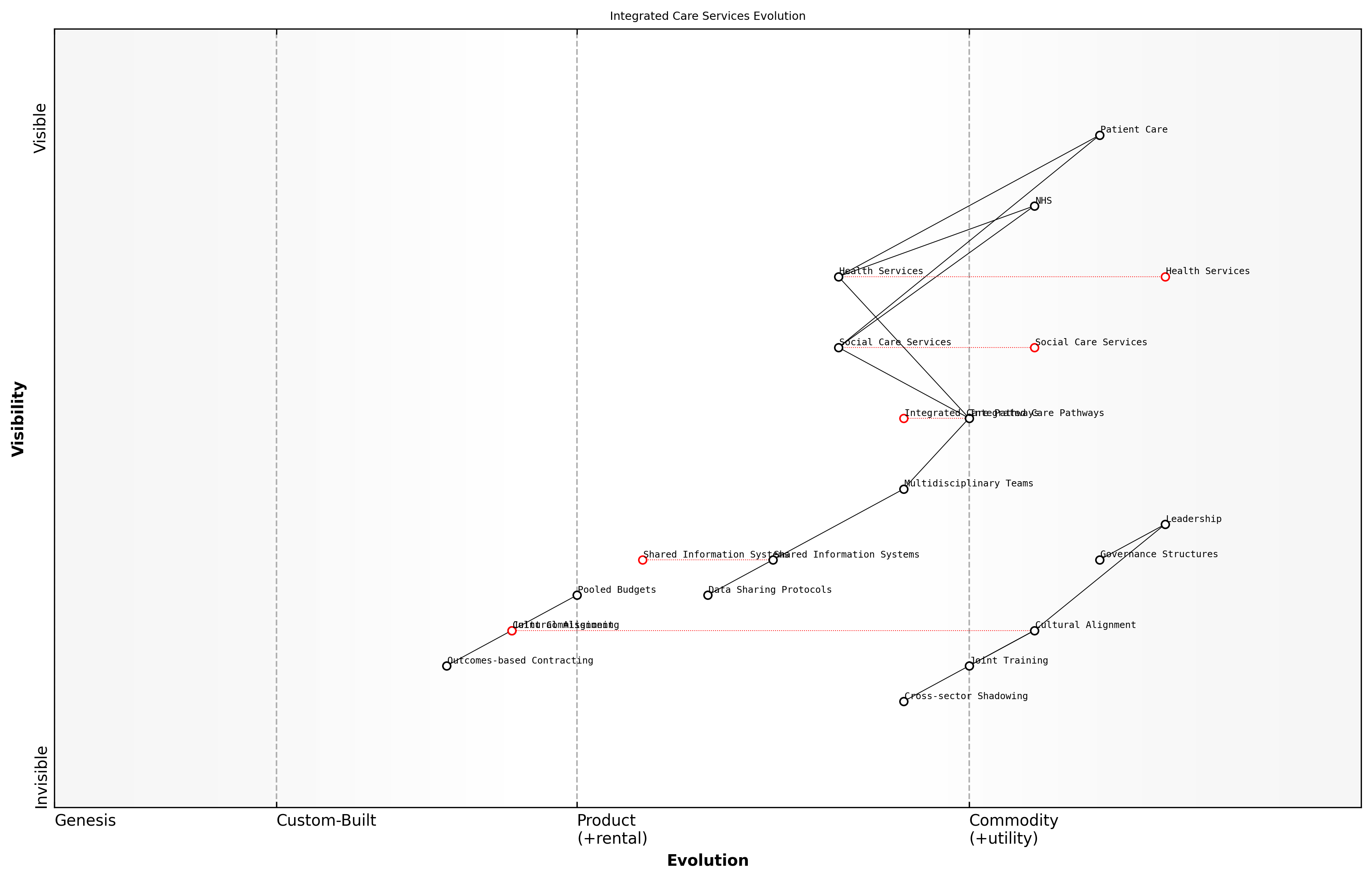
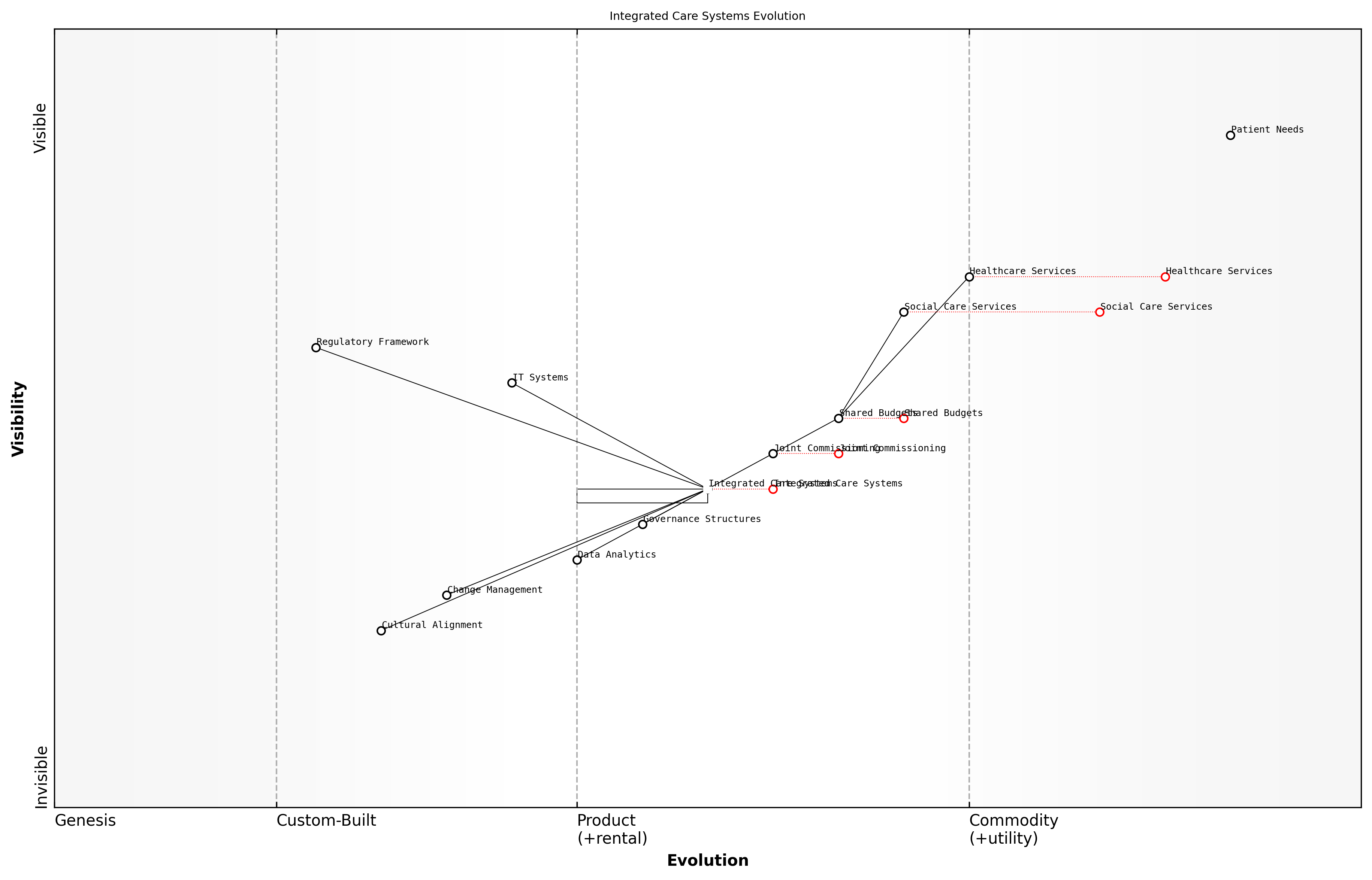
The integration of health and social care represents another systemic challenge for the NHS. The current fragmentation between these sectors leads to inefficiencies, gaps in care, and poor outcomes, particularly for older people and those with complex needs. While there have been efforts to promote integration, progress has been slow and uneven across the country.
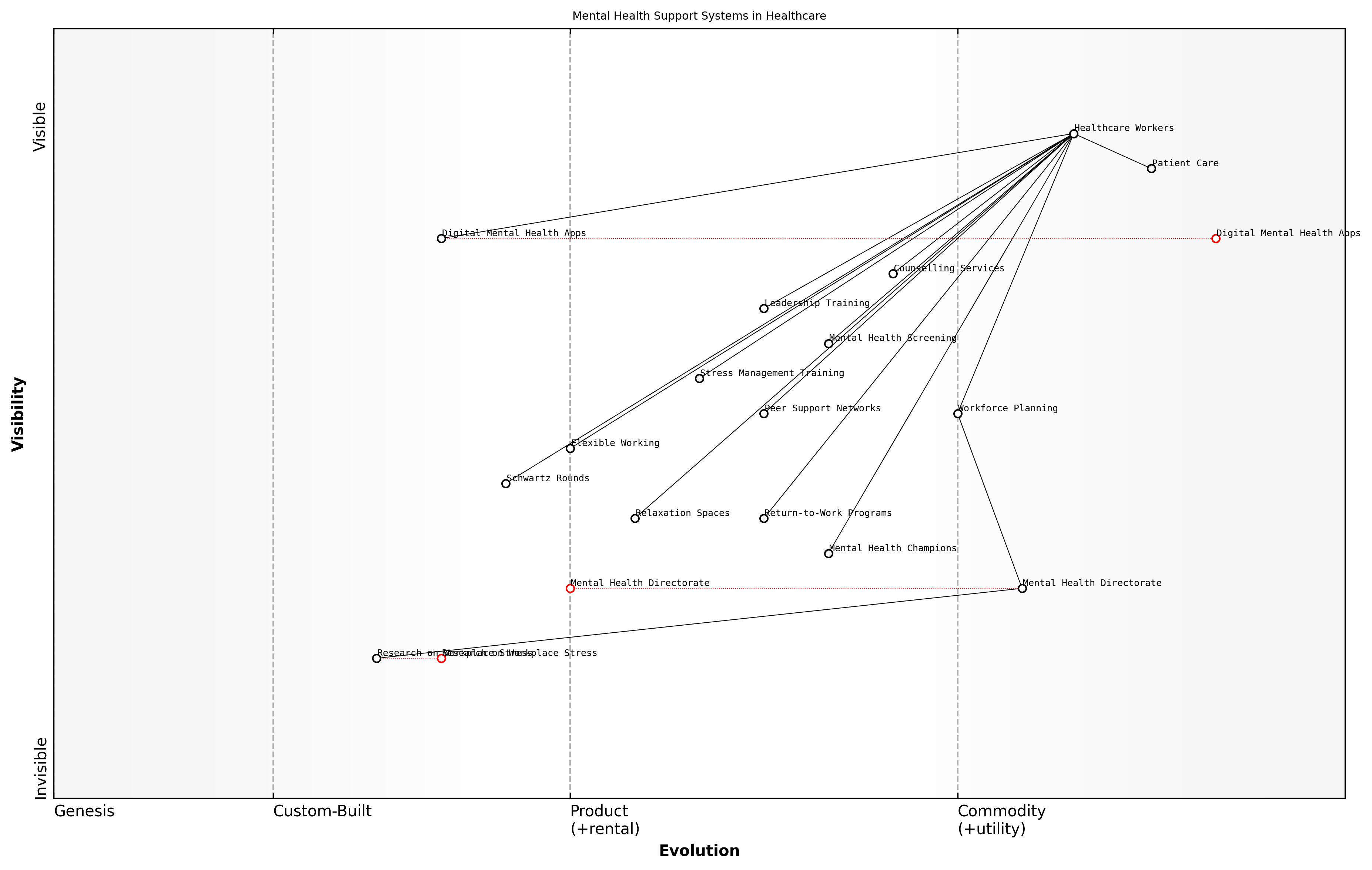
Mental health services within the NHS face particular pressures, with demand far outstripping capacity in many areas. Despite increased recognition of the importance of mental health and commitments to parity of esteem with physical health, mental health services continue to be stretched thin, with long waiting times for treatment and gaps in provision.
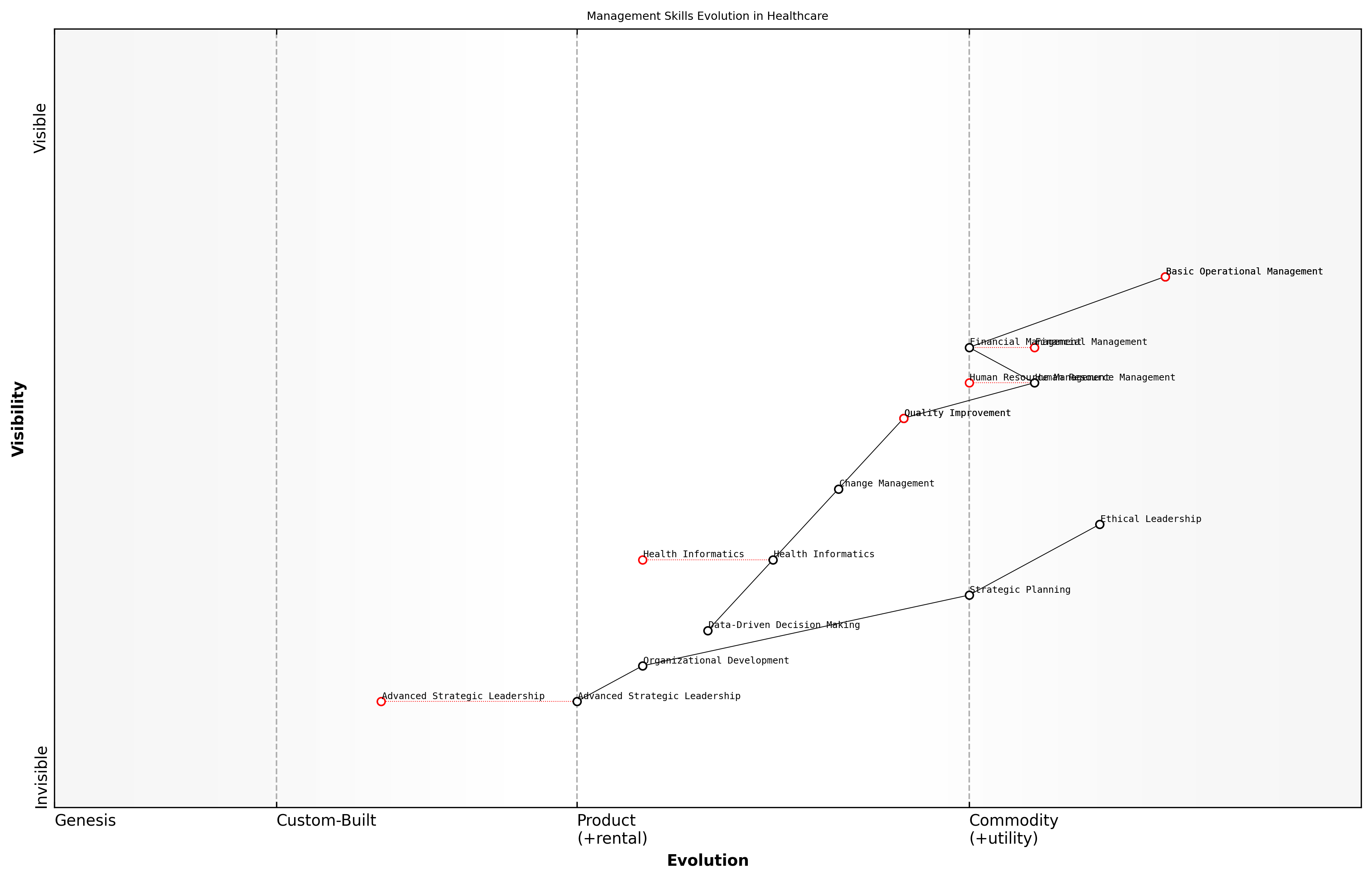
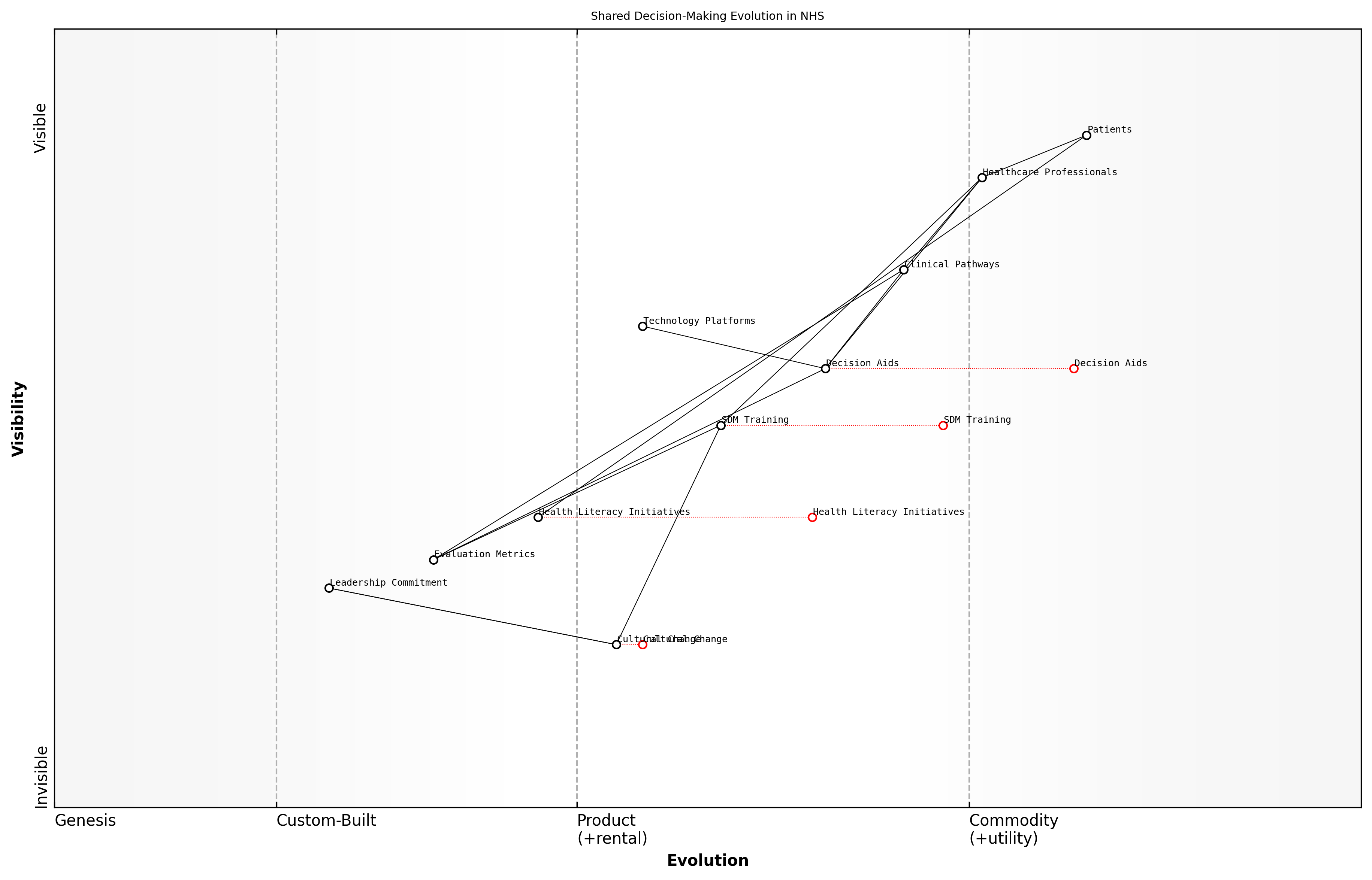
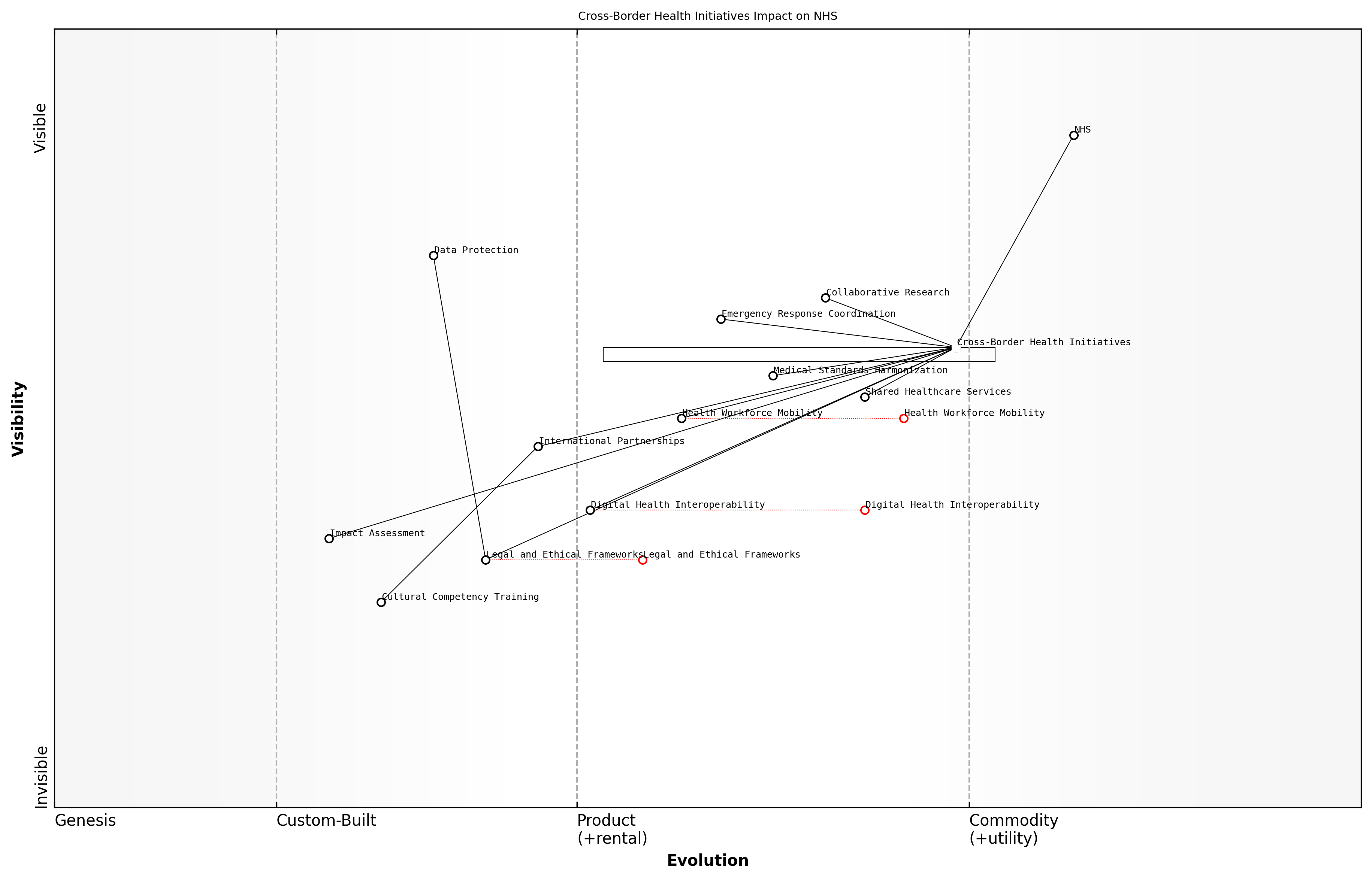
Wardley Map Assessment
The NHS faces significant pressures from demographic changes, resource constraints, and evolving healthcare needs. While it has strong foundations in healthcare delivery, it must navigate a complex transition towards more integrated, digitally-enabled care models. Success will depend on balancing short-term service pressures with long-term transformation, requiring strategic investments in workforce, technology, and new care models. The prominence of components like Health Inequalities and Health and Social Care Integration suggests a holistic approach to healthcare is emerging, which could position the NHS as a leader in comprehensive, equitable healthcare delivery if executed effectively.
[View full Wardley Map report](markdown/wardley_map_reports/wardley_map_report_02_english_Present-day Pressures and Systemic Issues.md)
The COVID-19 pandemic has both highlighted and exacerbated many of these existing pressures and systemic issues within the NHS. While the service's response to the crisis demonstrated its resilience and adaptability, the pandemic has also left a legacy of increased backlogs, staff burnout, and the need for long-term recovery planning.
In conclusion, the NHS faces a complex web of interrelated pressures and systemic issues that require urgent attention. Addressing these challenges will require not only increased resources but also innovative approaches to service delivery, workforce management, and system integration. The future sustainability and effectiveness of the NHS depend on our ability to tackle these issues head-on, with a clear vision for reform and a commitment to preserving the core principles of universal, high-quality healthcare for all.
The Urgent Need for Transformation
The National Health Service (NHS) stands at a critical juncture, facing unprecedented challenges that demand urgent and comprehensive transformation. As an expert who has closely studied and advised on NHS reform for over two decades, I can attest that the need for change has never been more pressing. The confluence of demographic shifts, technological advancements, and evolving healthcare demands has created a perfect storm that threatens the very foundations of this beloved institution.
The NHS, once a beacon of universal healthcare, now grapples with systemic issues that undermine its ability to deliver on its founding principles. Long waiting times, resource constraints, and an overburdened workforce have become the norm rather than the exception. The COVID-19 pandemic has further exposed and exacerbated these underlying weaknesses, pushing the system to its breaking point and highlighting the urgent need for radical reform.
- Unsustainable financial pressures due to an ageing population and rising costs of medical technologies
- Workforce shortages and burnout, leading to compromised patient care and staff retention issues
- Outdated infrastructure and digital systems ill-equipped to meet modern healthcare demands
- Growing health inequalities that challenge the NHS's core principle of equitable access to care
- Increasing prevalence of chronic diseases requiring complex, long-term management
The urgency of transformation is underscored by the stark reality that without significant change, the NHS risks becoming obsolete in the face of 21st-century healthcare challenges. We must act now to preserve the essence of the NHS while reimagining its structure and operations to ensure sustainability and effectiveness in the years to come.
The NHS is facing its greatest challenge since its inception. We must embrace transformation not as a choice, but as an imperative for survival and future excellence in healthcare delivery.
Transformation must be holistic, addressing not only the immediate crises but also laying the groundwork for a resilient, adaptive healthcare system. This involves rethinking every aspect of the NHS, from its funding models and workforce strategies to its use of technology and approach to patient care. The transformation agenda must balance the need for rapid change with the importance of maintaining the NHS's core values of universality and equity.
Key areas requiring immediate attention include:
- Embracing digital health technologies to improve efficiency and access to care
- Implementing data-driven decision-making processes to optimise resource allocation
- Developing innovative workforce models to address staffing shortages and improve job satisfaction
- Redesigning care pathways to focus on prevention and community-based interventions
- Exploring new funding mechanisms to ensure long-term financial sustainability
The urgency of transformation also necessitates a shift in mindset among all stakeholders. Political leaders must move beyond short-term fixes and commit to long-term, systemic change. Healthcare professionals must be empowered to drive innovation from within the system. Patients and the public must be engaged as active partners in shaping the future of their healthcare services.
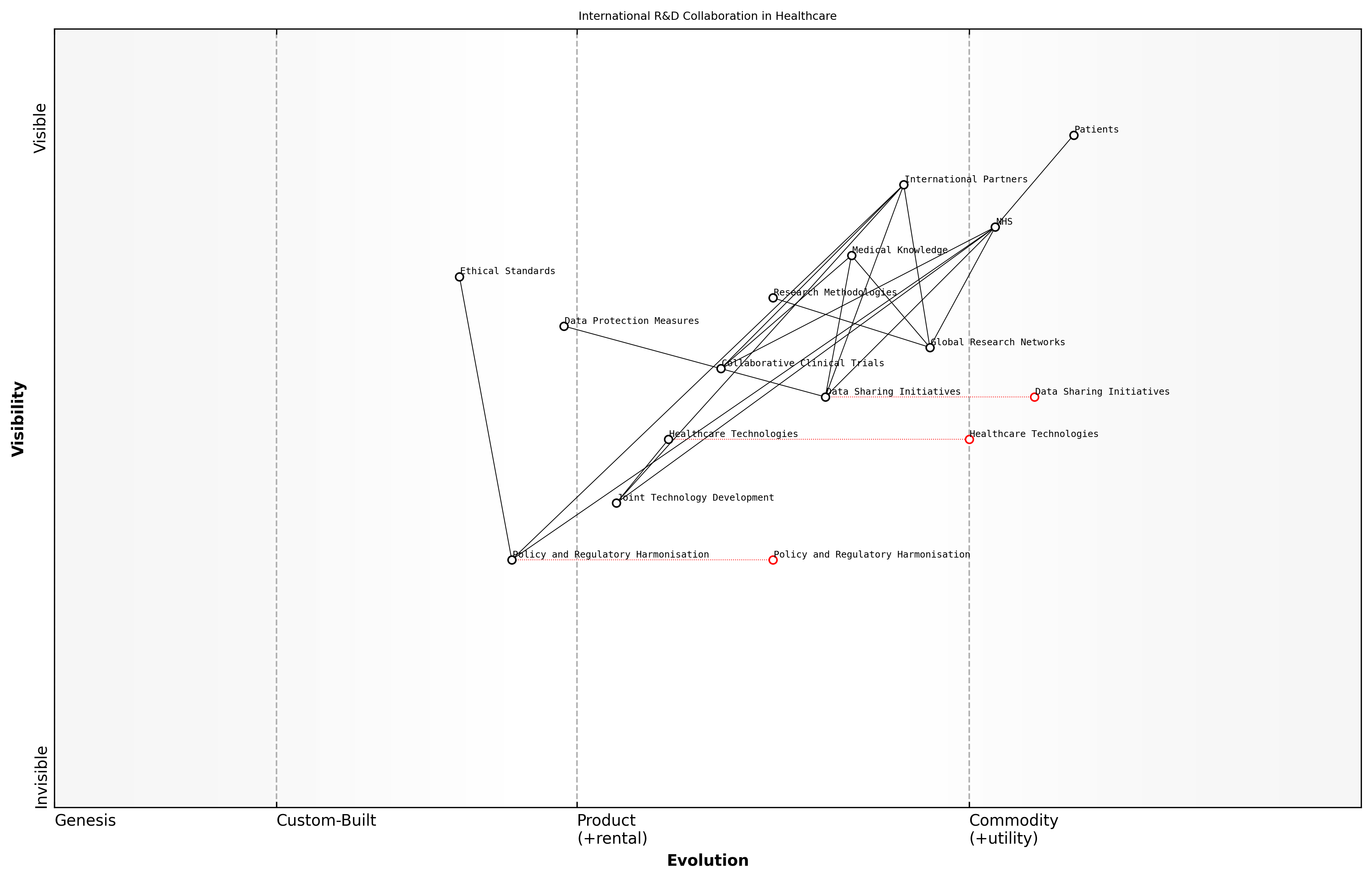
Wardley Map Assessment
The NHS is at a critical juncture, facing urgent need for transformation. While core strengths in healthcare delivery and values remain, significant evolution is required in digital technologies, data-driven decision making, and workforce capabilities. Strategic focus on these areas, coupled with innovative funding models and care pathways, can position the NHS to meet future healthcare demands effectively.
[View full Wardley Map report](markdown/wardley_map_reports/wardley_map_report_03_english_The Urgent Need for Transformation.md)
As we embark on this transformative journey, it is crucial to recognise that the process will be challenging and, at times, uncomfortable. However, the cost of inaction far outweighs the difficulties of change. The NHS has always been a source of national pride and a model for healthcare systems worldwide. By embracing urgent transformation, we have the opportunity to not only save this vital institution but to reinvent it as a beacon of innovation and excellence in healthcare for the 21st century and beyond.
The transformation of the NHS is not just about preserving a system; it's about safeguarding the health and well-being of generations to come. We owe it to ourselves and to future generations to act decisively and courageously.
In conclusion, the urgent need for transformation in the NHS is clear and inescapable. As we delve deeper into the specific areas of reform in subsequent chapters, it is imperative to keep this sense of urgency at the forefront of our minds. The future of healthcare in the UK depends on our ability to rise to this challenge and effect meaningful, lasting change.
A Vision for a Revitalized NHS
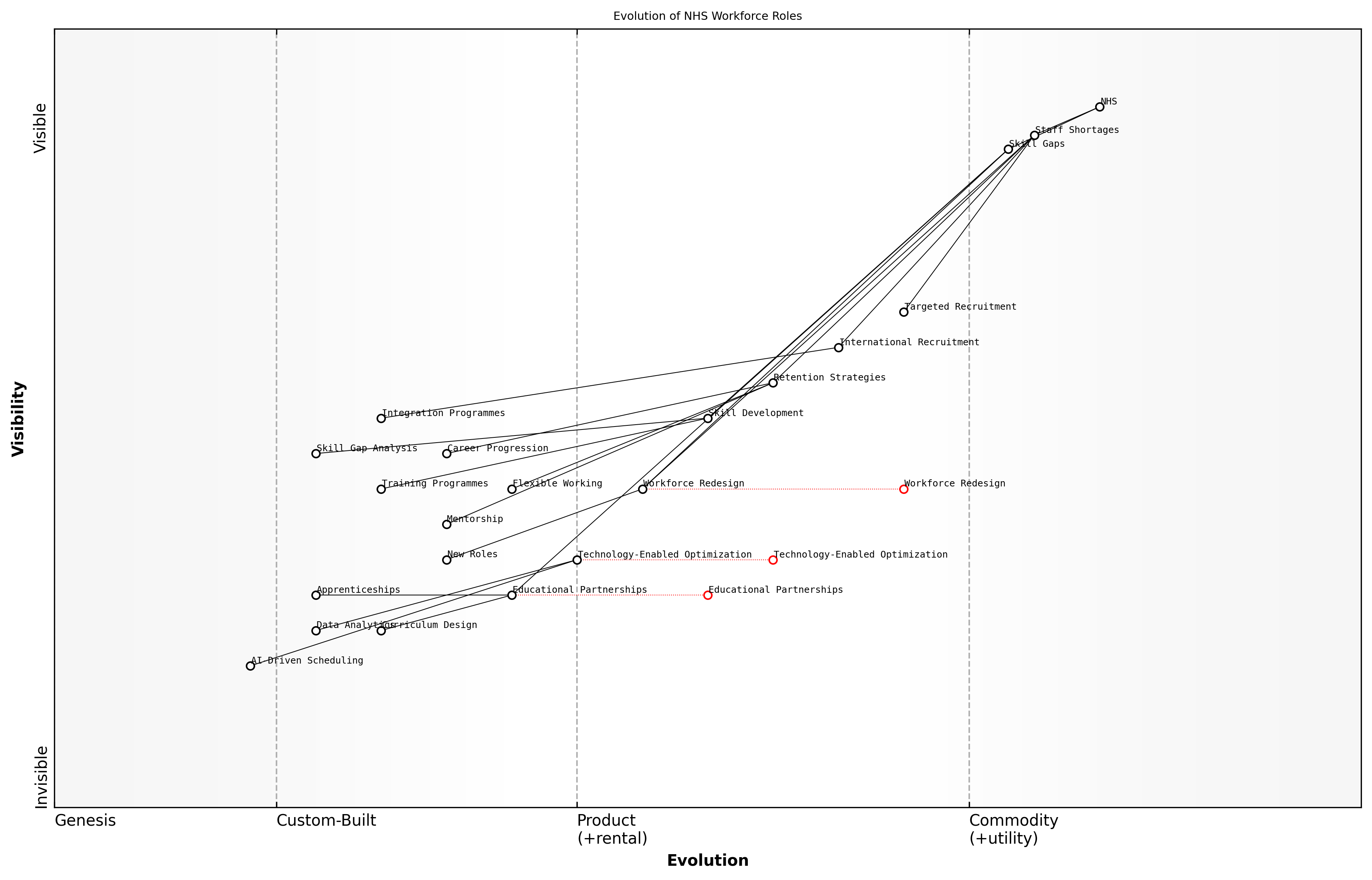
Key Areas for Reform
As we envision a revitalised National Health Service (NHS), it is crucial to identify and prioritise key areas for reform. These areas represent the critical pillars upon which a sustainable, efficient, and patient-centric healthcare system can be built. Drawing from decades of experience in healthcare policy and reform, I can confidently assert that addressing these key areas will not only alleviate current pressures but also future-proof the NHS against emerging challenges.
- Digital Transformation and Data Utilisation
- Workforce Optimisation and Well-being
- Patient-Centred Care Models
- Sustainable Funding and Resource Allocation
- Cross-Sector Collaboration and Integration
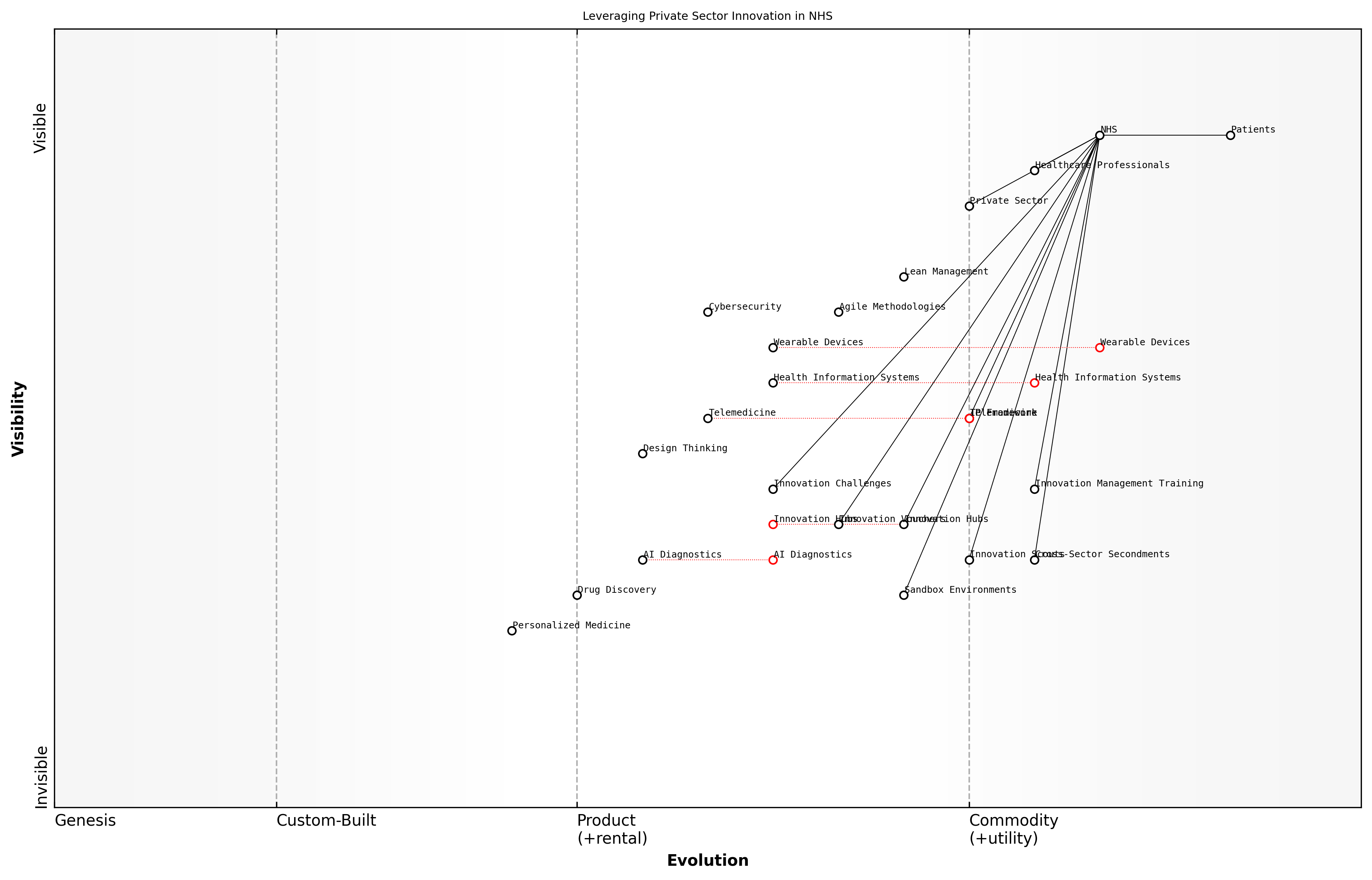
Digital Transformation and Data Utilisation stands at the forefront of NHS reform. The integration of advanced health informatics systems, telemedicine, and artificial intelligence can revolutionise care delivery, improve diagnostic accuracy, and enhance resource allocation. However, this transformation must be underpinned by robust data governance frameworks and strategies to bridge the digital divide, ensuring equitable access to digital health solutions across all demographics.
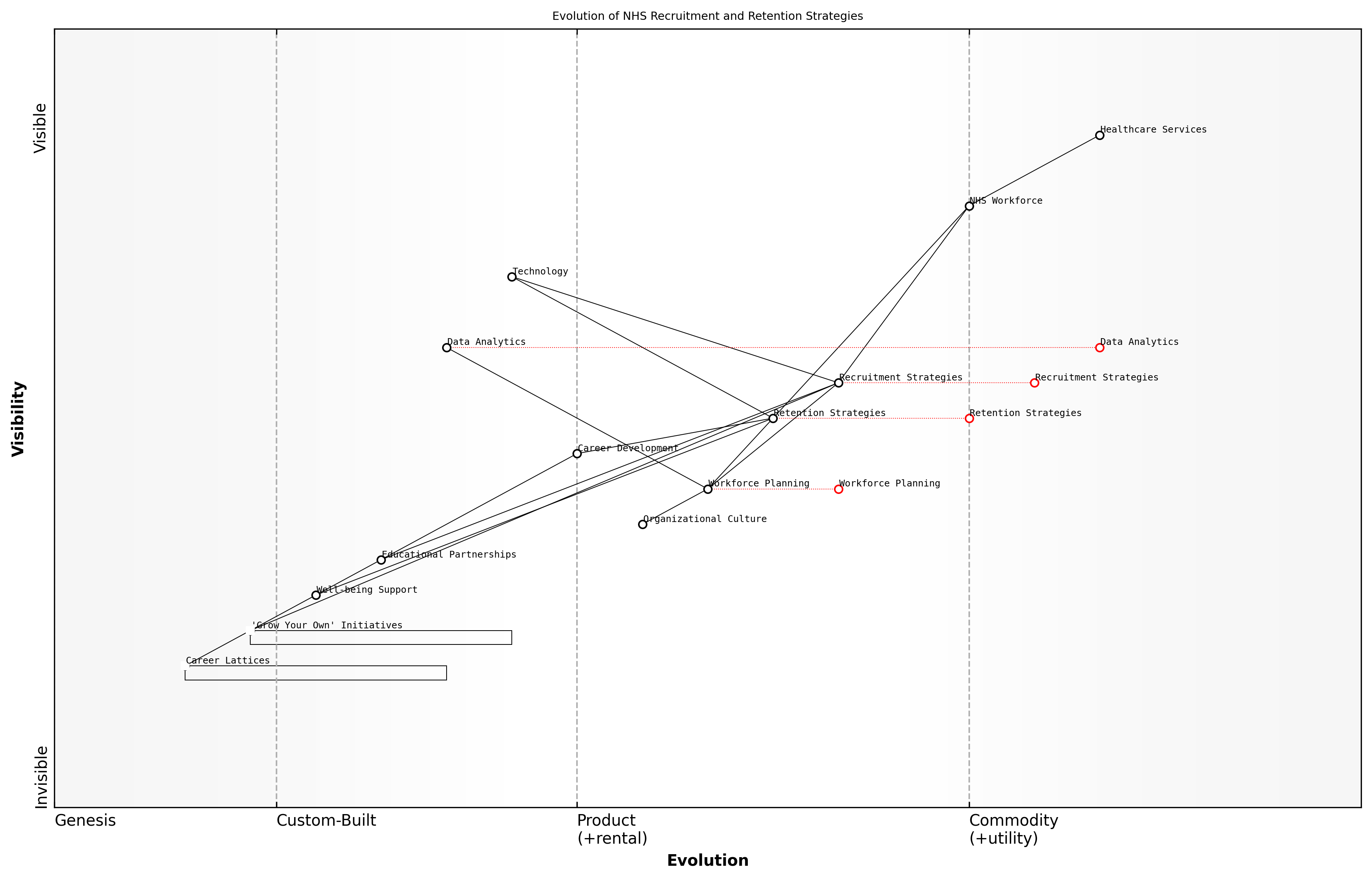
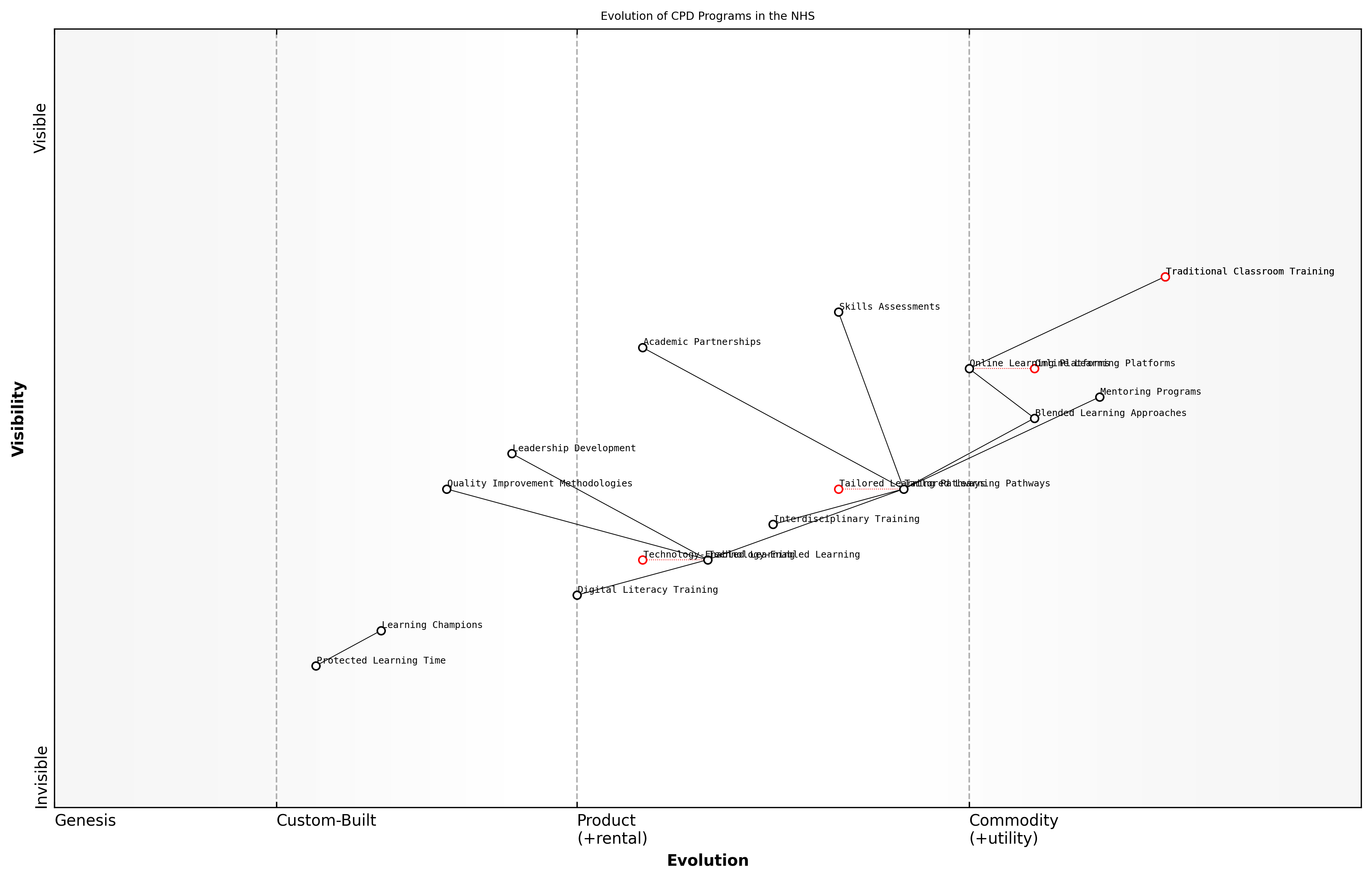
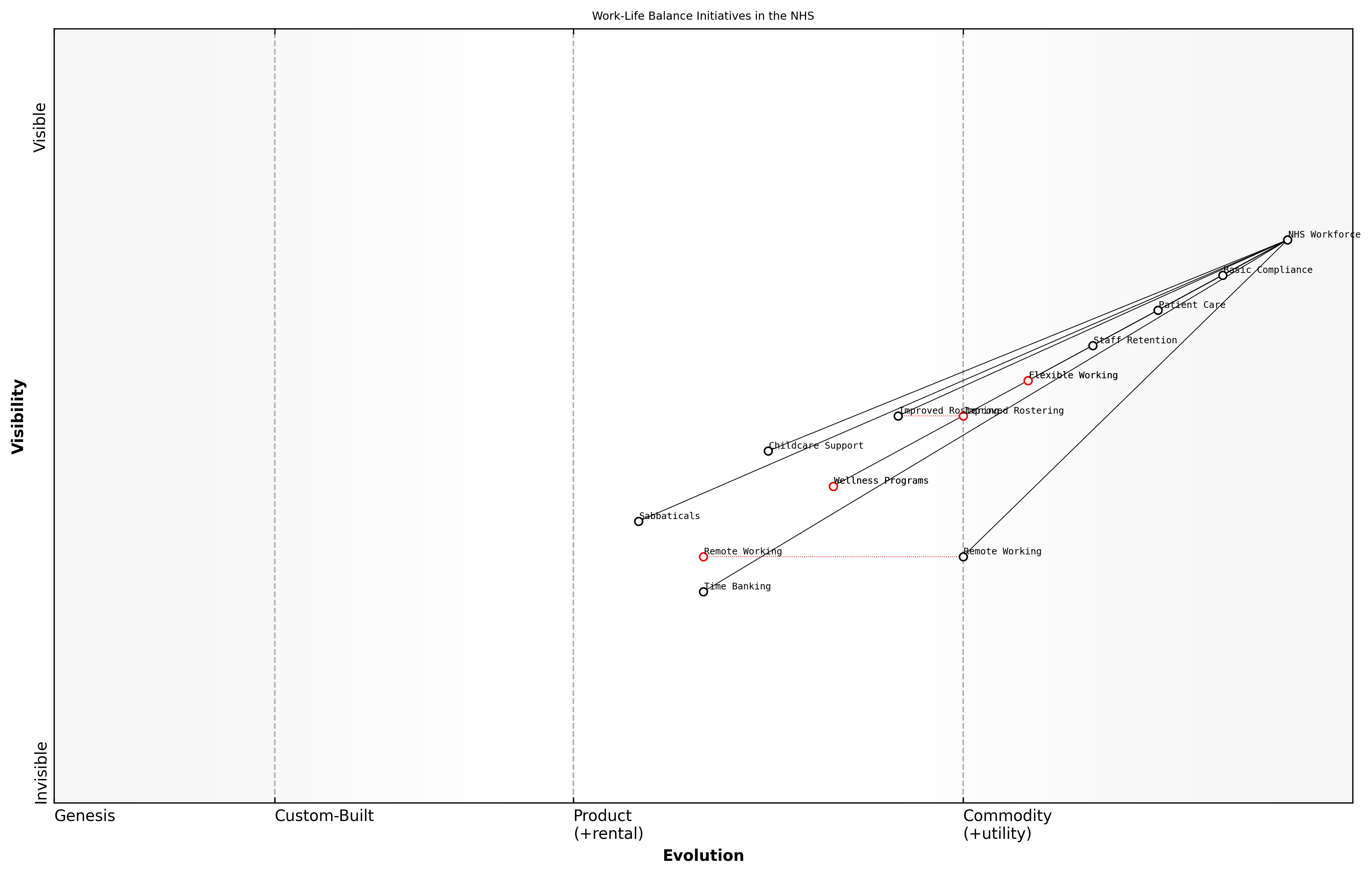
Workforce Optimisation and Well-being is paramount in addressing the chronic staffing shortages and burnout issues plaguing the NHS. This area of reform encompasses innovative recruitment strategies, continuous professional development programmes, and initiatives to improve work-life balance and mental health support for healthcare workers. By nurturing a resilient and satisfied workforce, we can ensure the delivery of high-quality care and reduce costly staff turnover.
A healthcare system is only as strong as its workforce. Investing in our staff is not just a moral imperative, but a financial necessity for the long-term sustainability of the NHS.
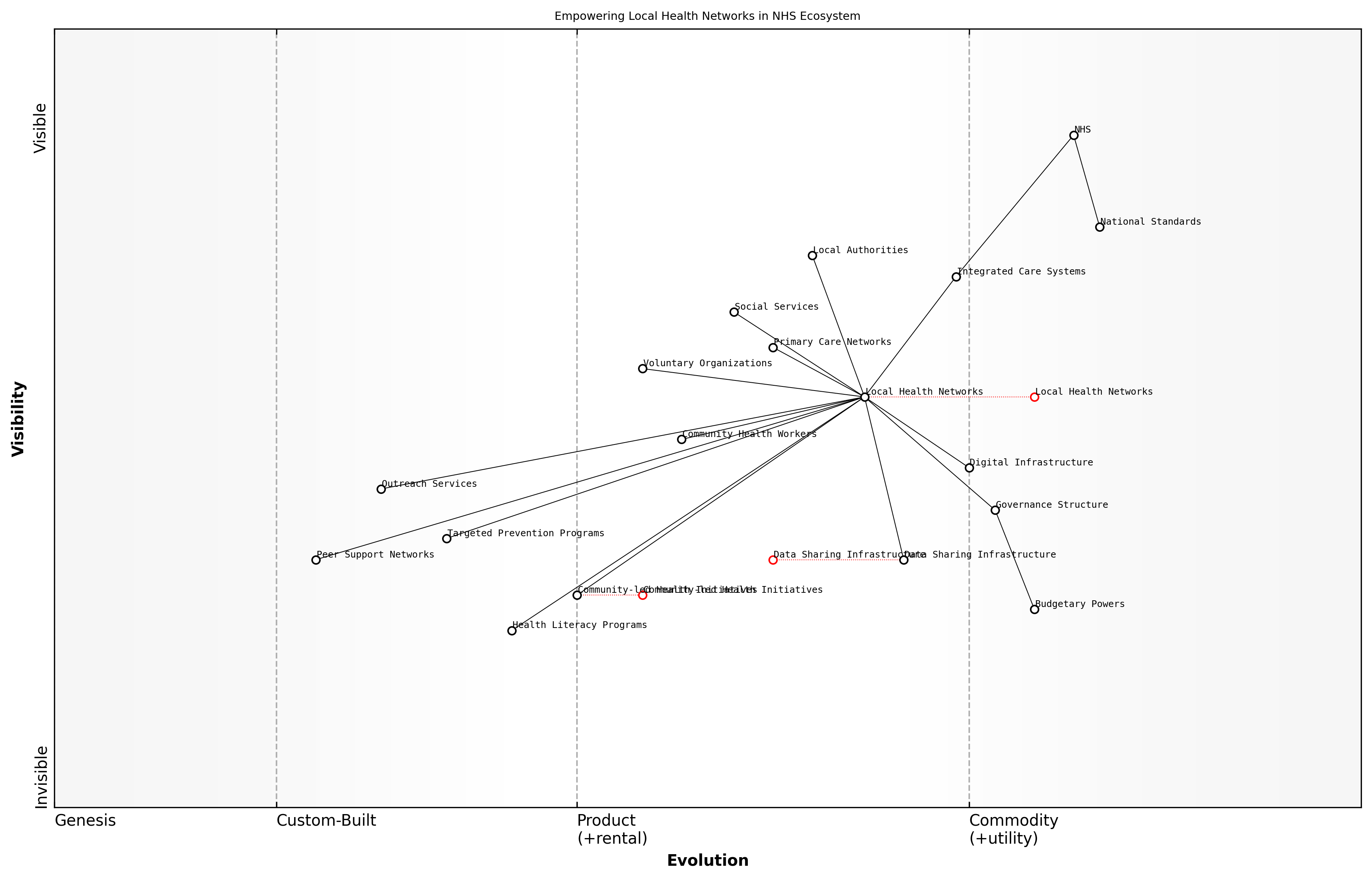
Patient-Centred Care Models represent a paradigm shift in how healthcare is conceptualised and delivered. This reform area focuses on personalised medicine, shared decision-making processes, and community health initiatives. By empowering patients and local health networks, we can improve health outcomes, increase patient satisfaction, and reduce the burden on acute care services through more effective preventive care and chronic disease management.
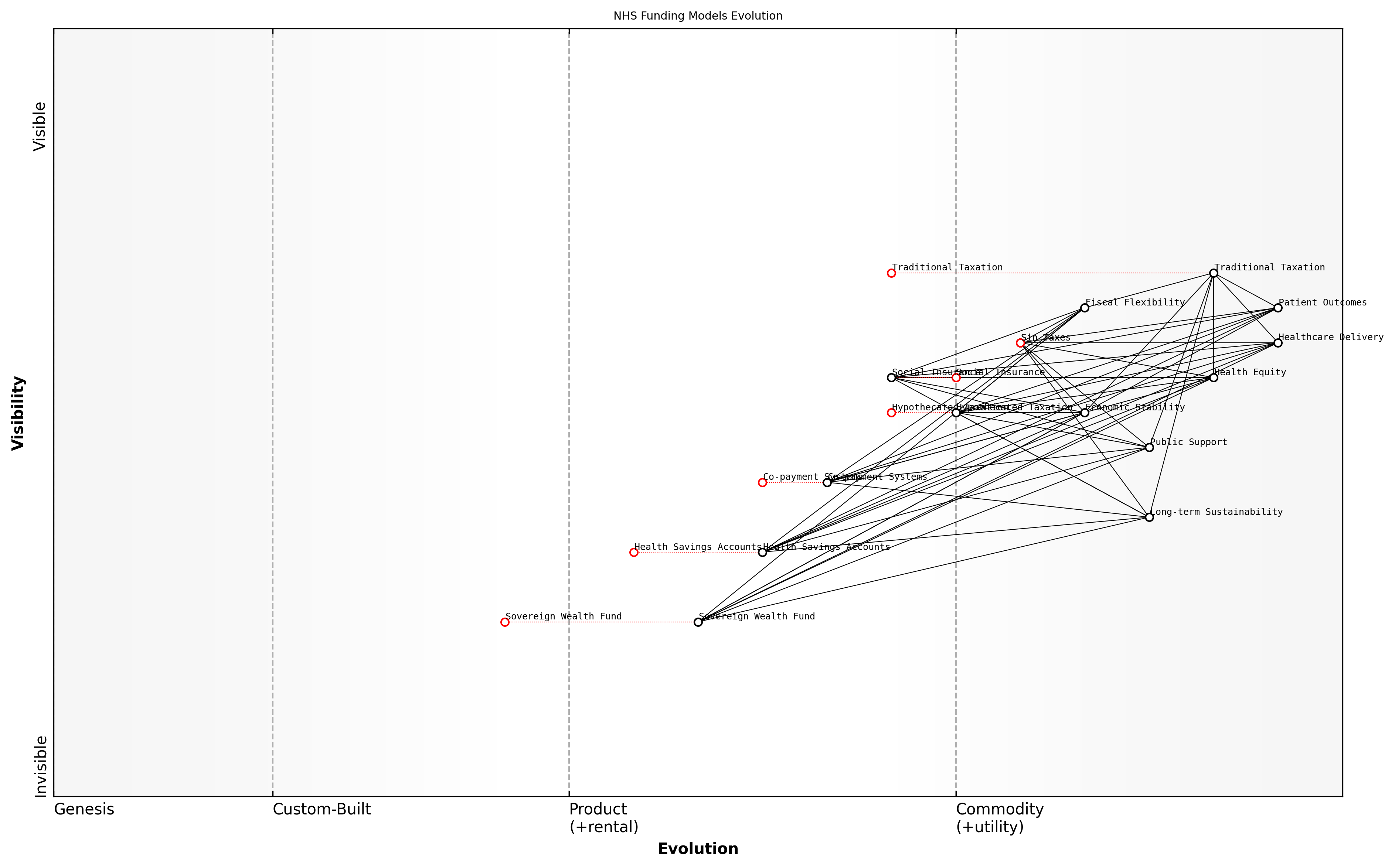
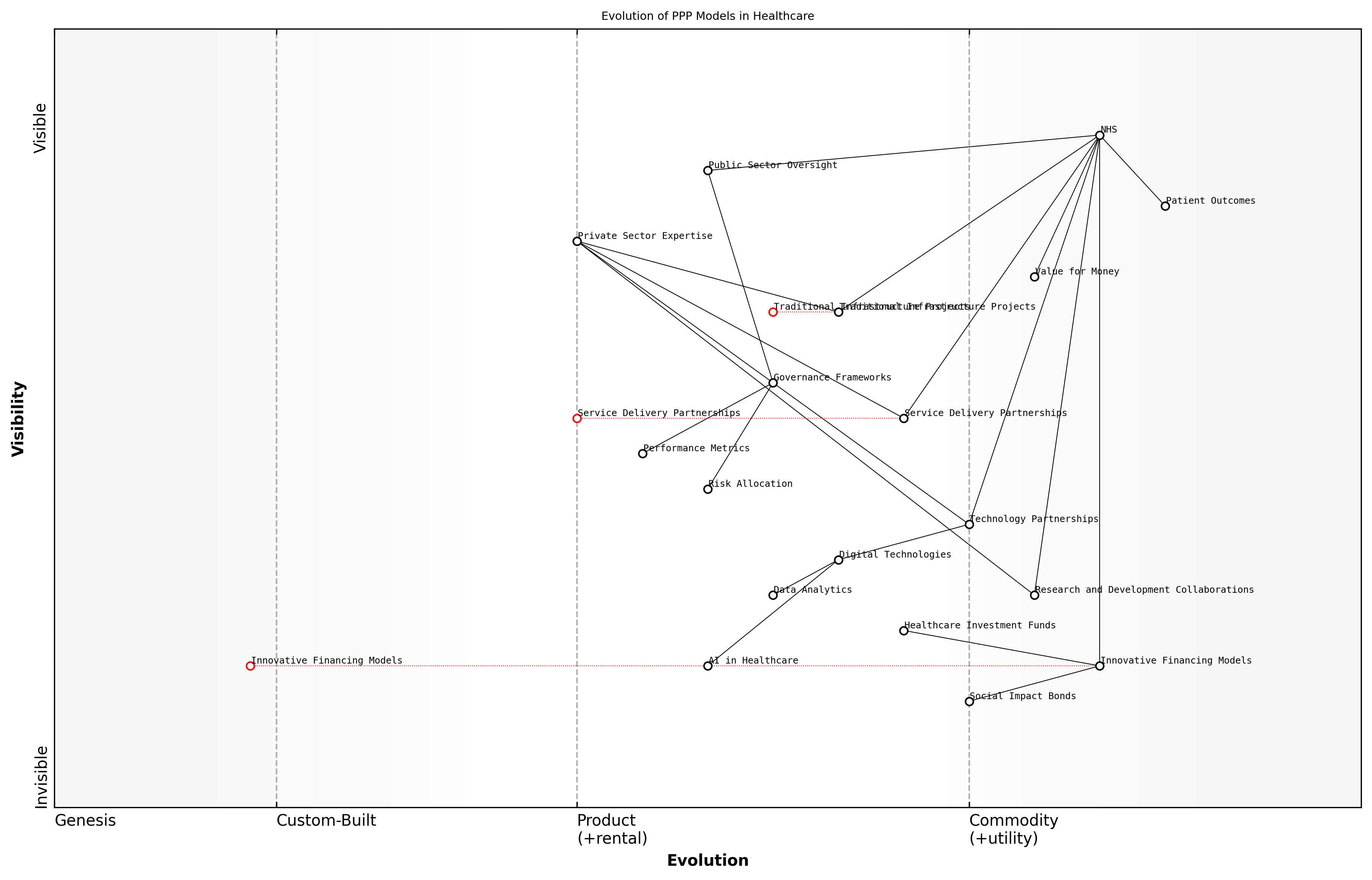
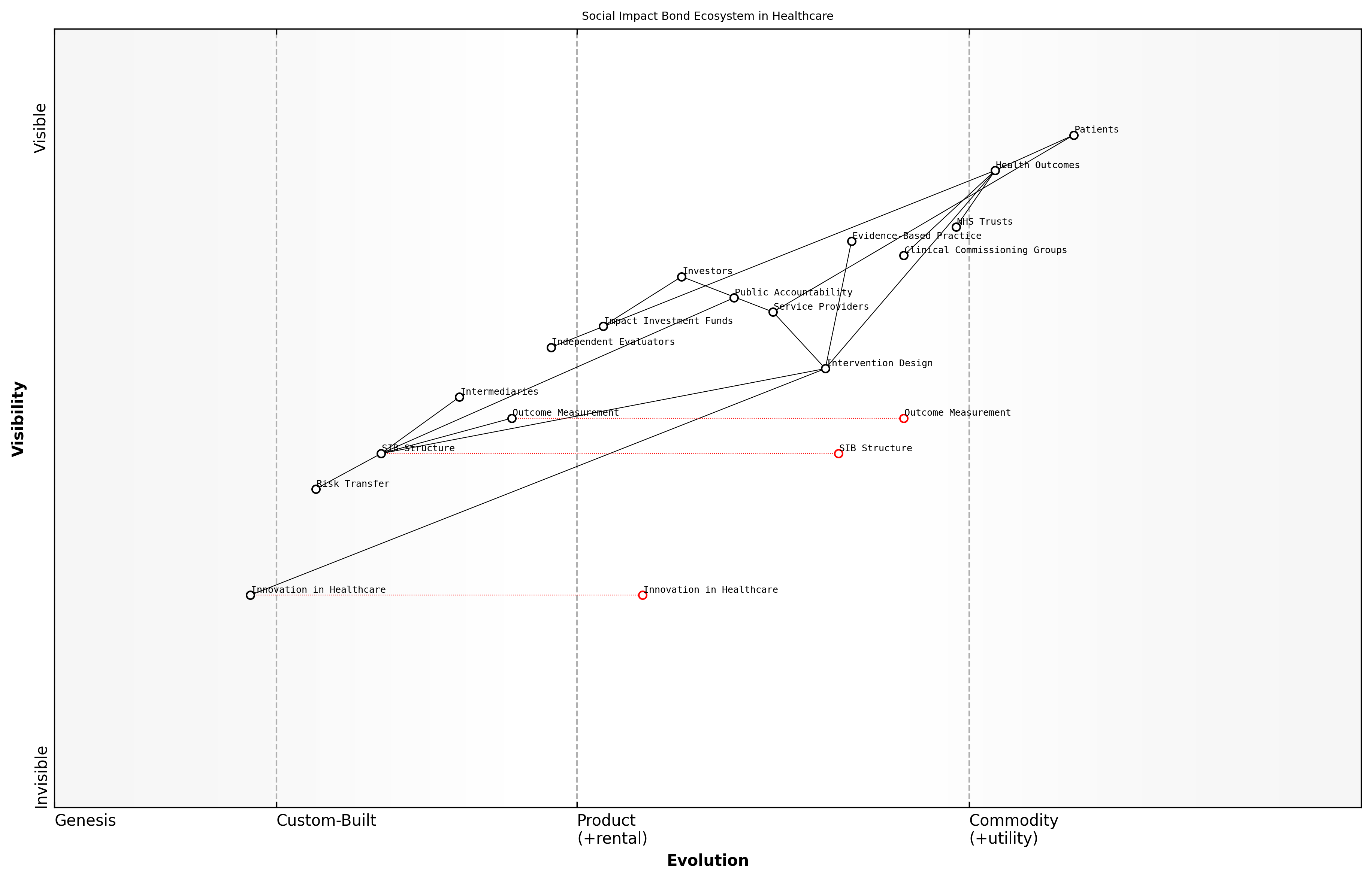
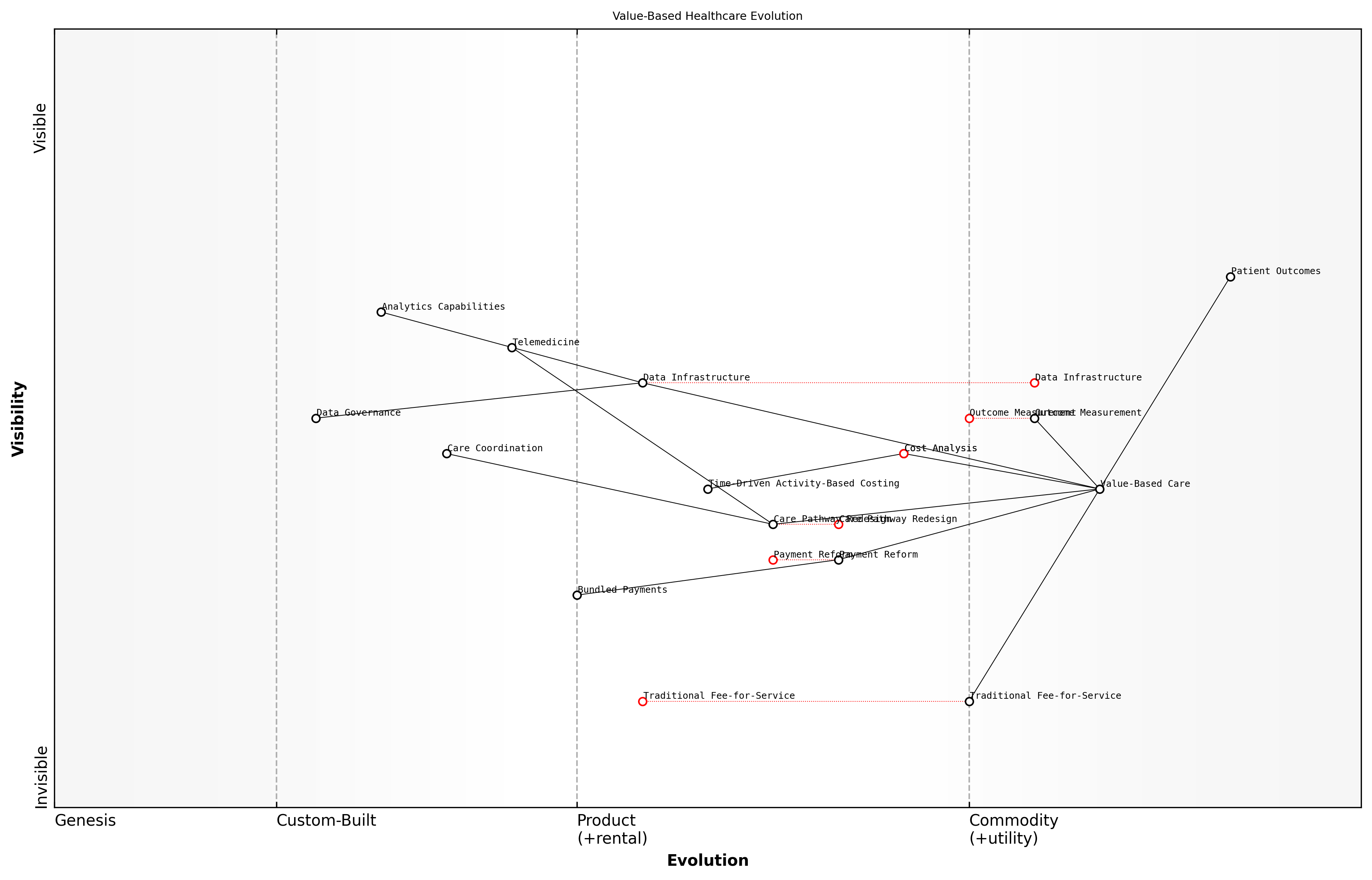
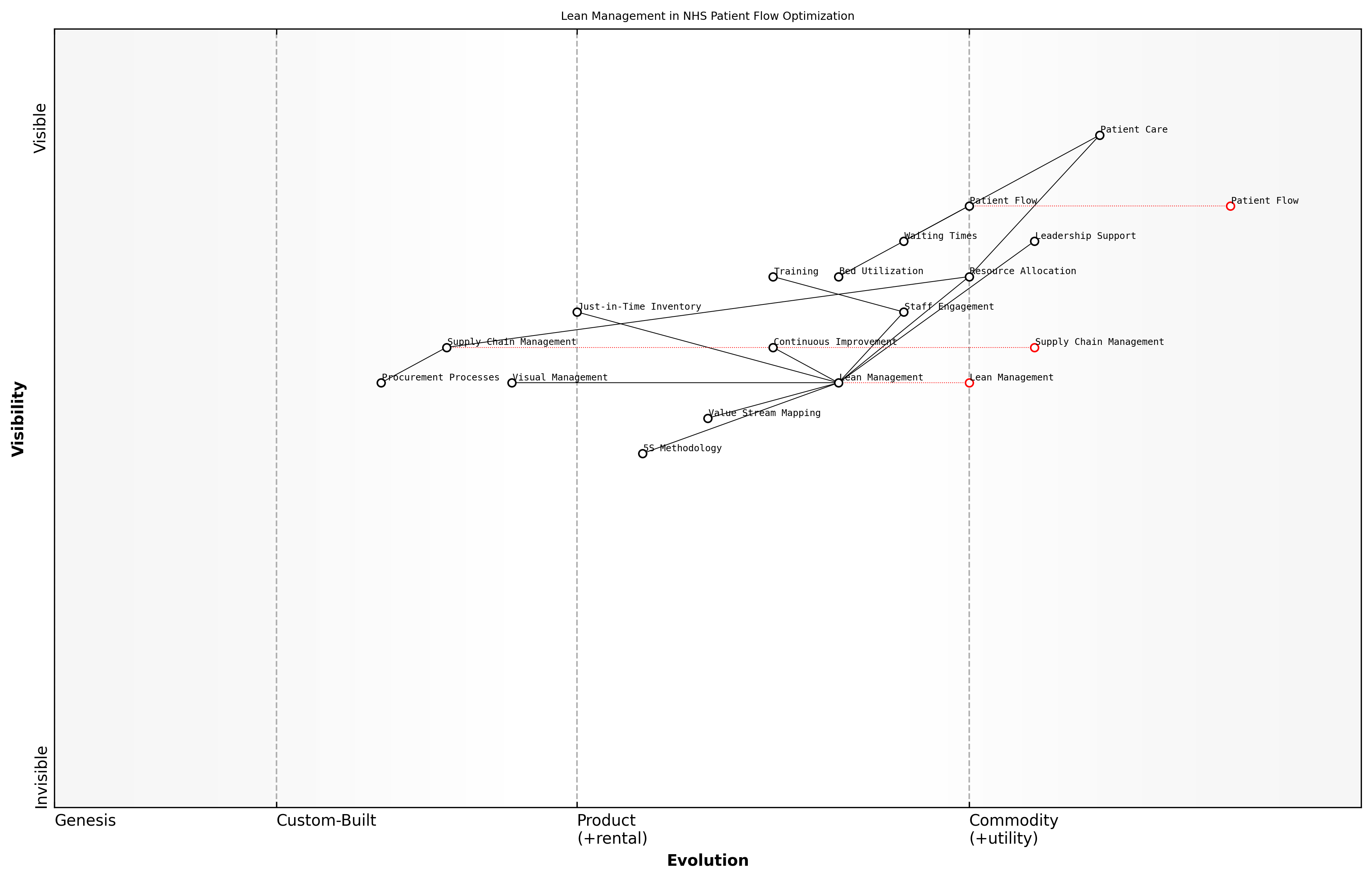
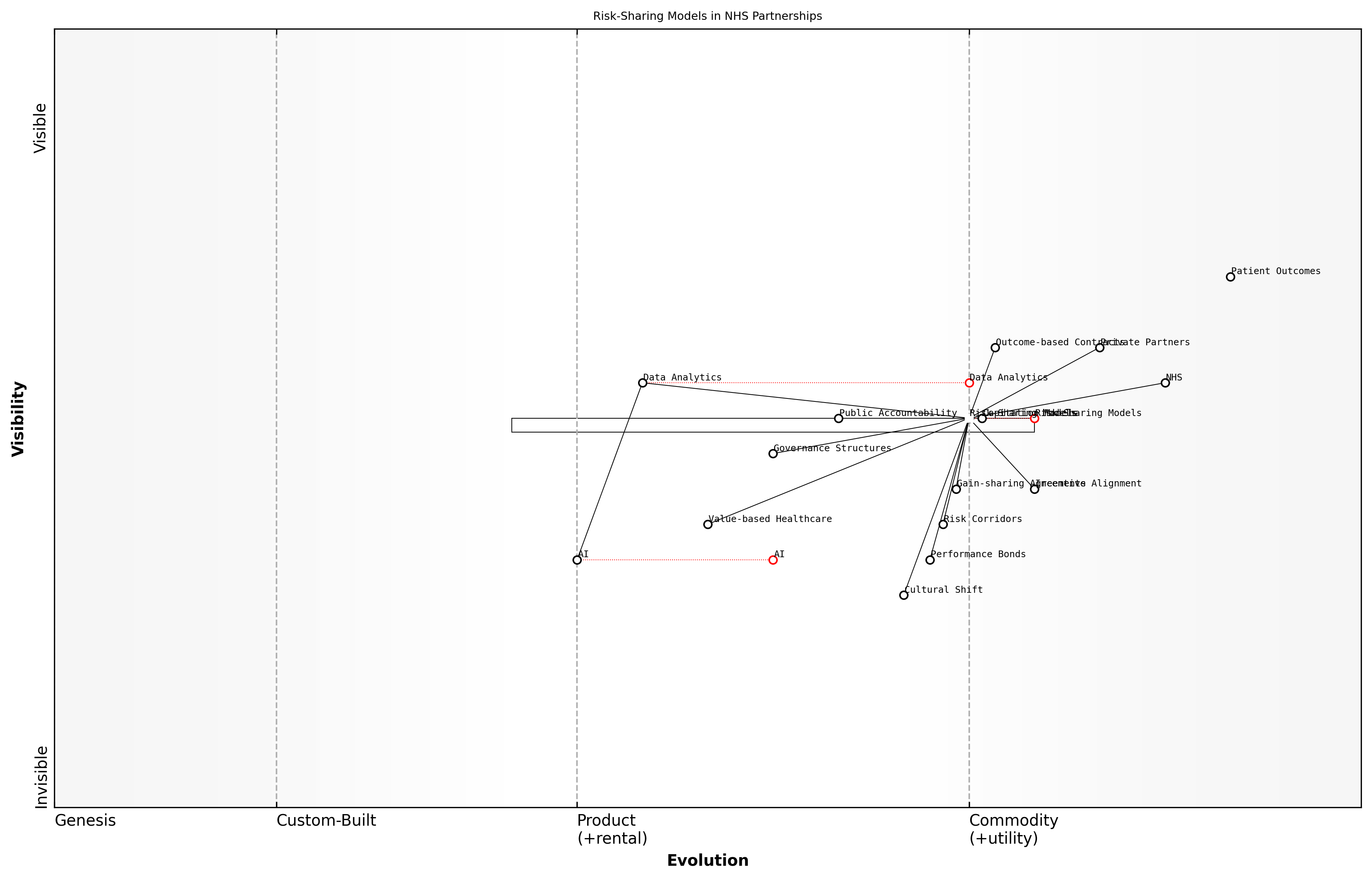
Sustainable Funding and Resource Allocation is critical for the NHS's long-term viability. This area of reform explores innovative funding mechanisms, such as social impact bonds and public-private partnerships, alongside efficiency-driven approaches like value-based healthcare and lean management principles. The goal is to ensure that the NHS can continue to provide universal coverage while maintaining fiscal responsibility in the face of increasing healthcare demands and costs.
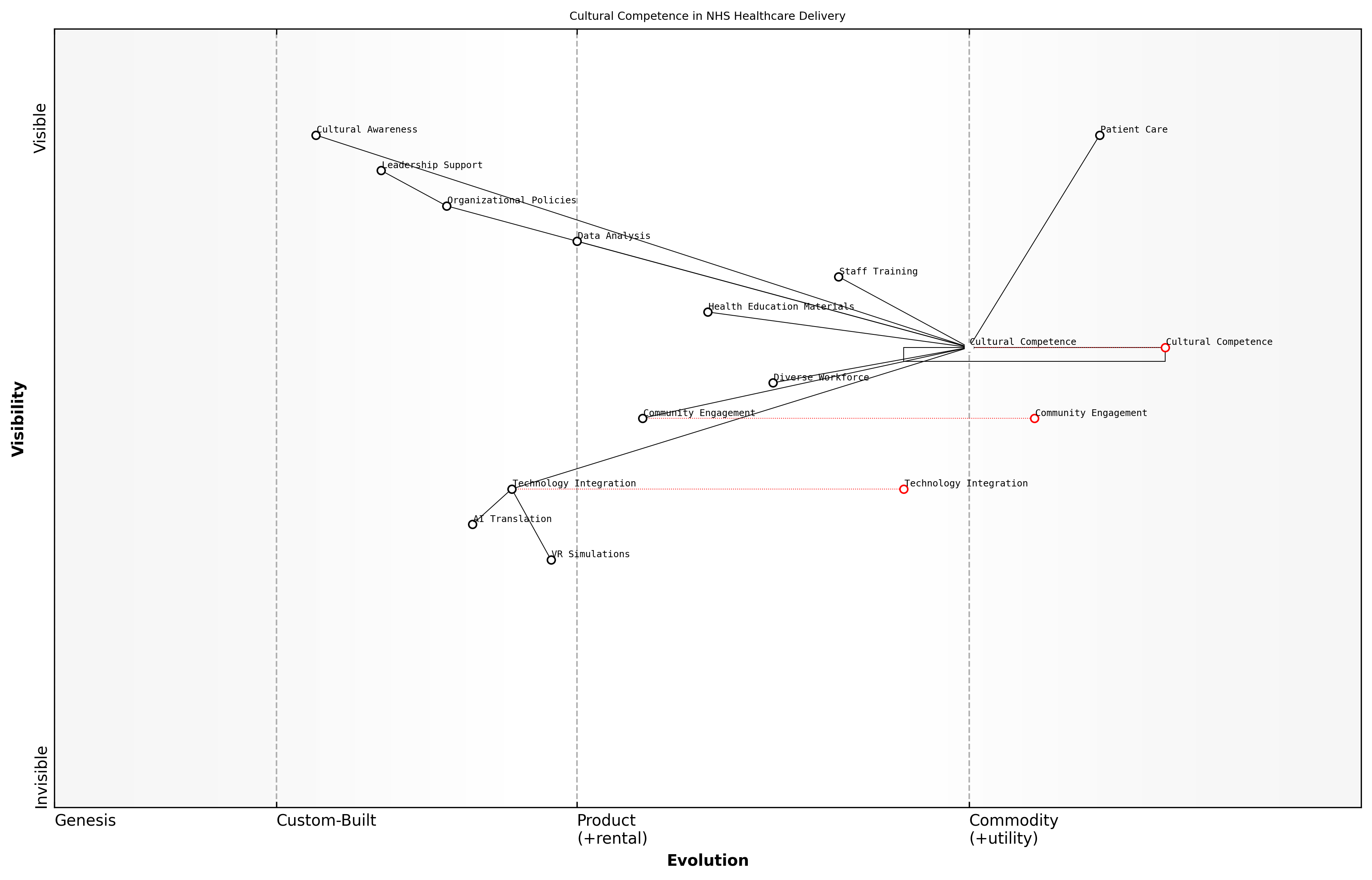
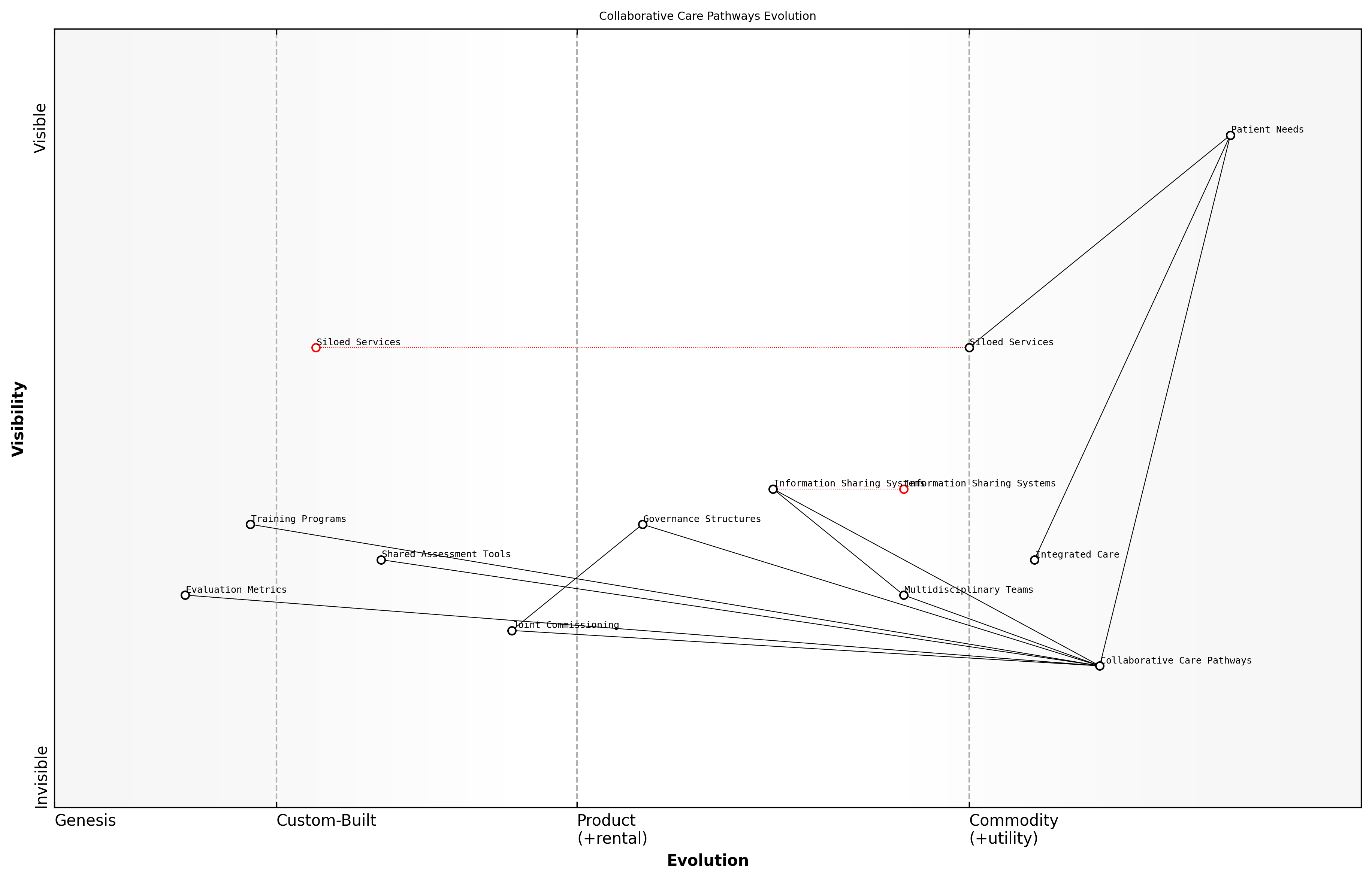
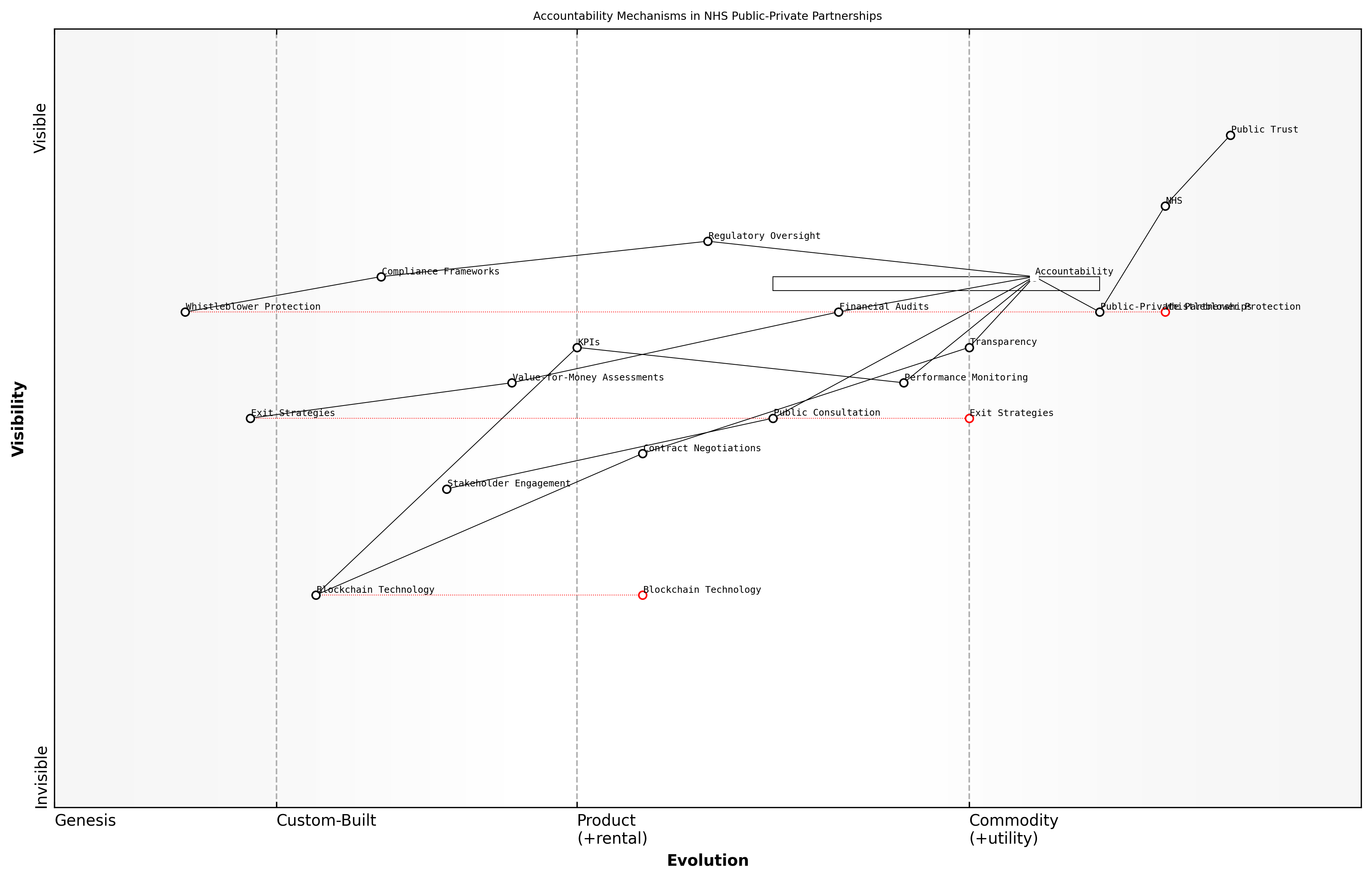
Cross-Sector Collaboration and Integration is essential for creating a holistic healthcare ecosystem. This reform area focuses on breaking down silos between health and social care, fostering public-private partnerships to drive innovation, and engaging in international knowledge exchange to adopt global best practices. By creating collaborative care pathways and shared accountability models, we can address complex health challenges more effectively and efficiently.
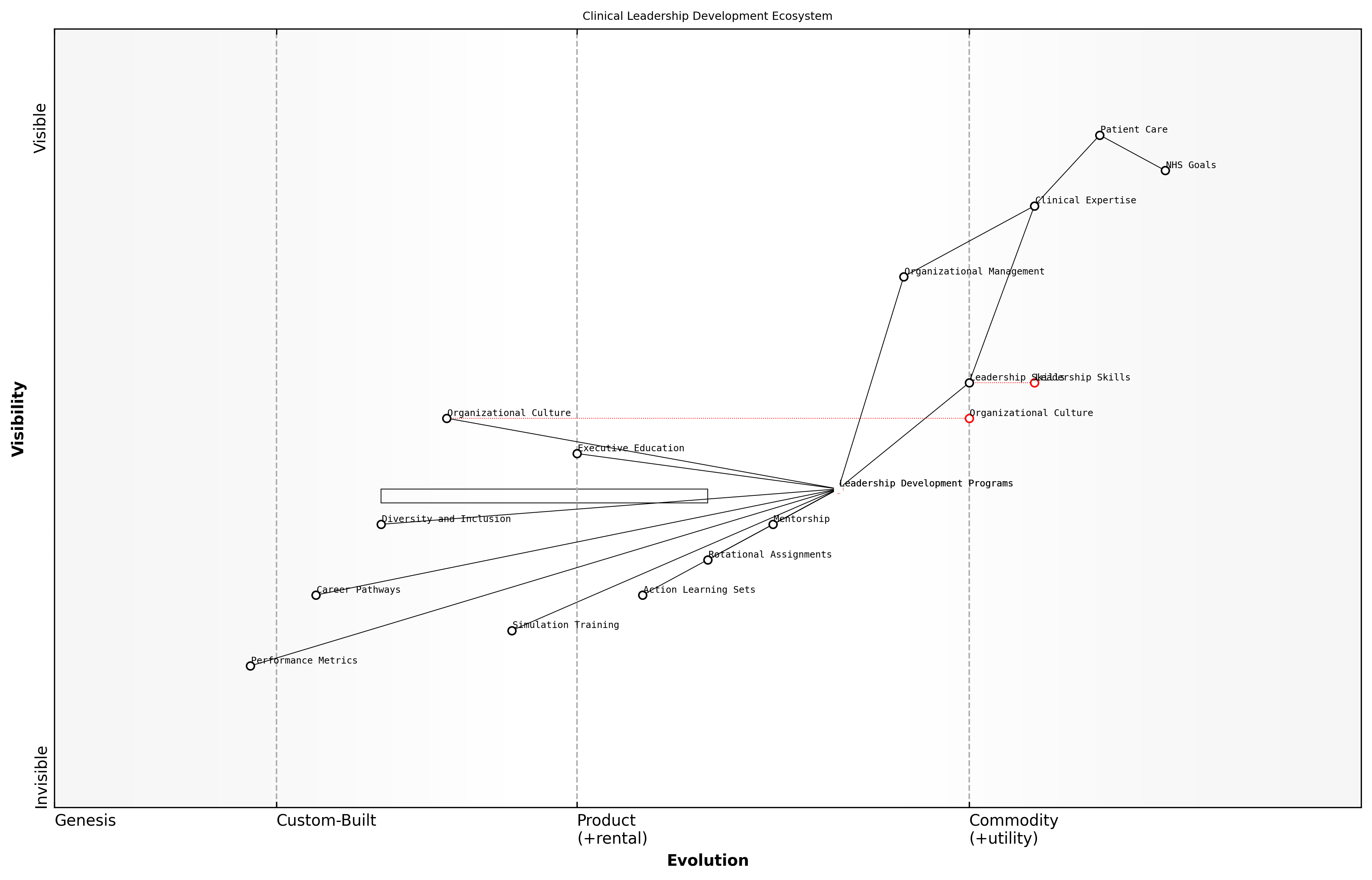
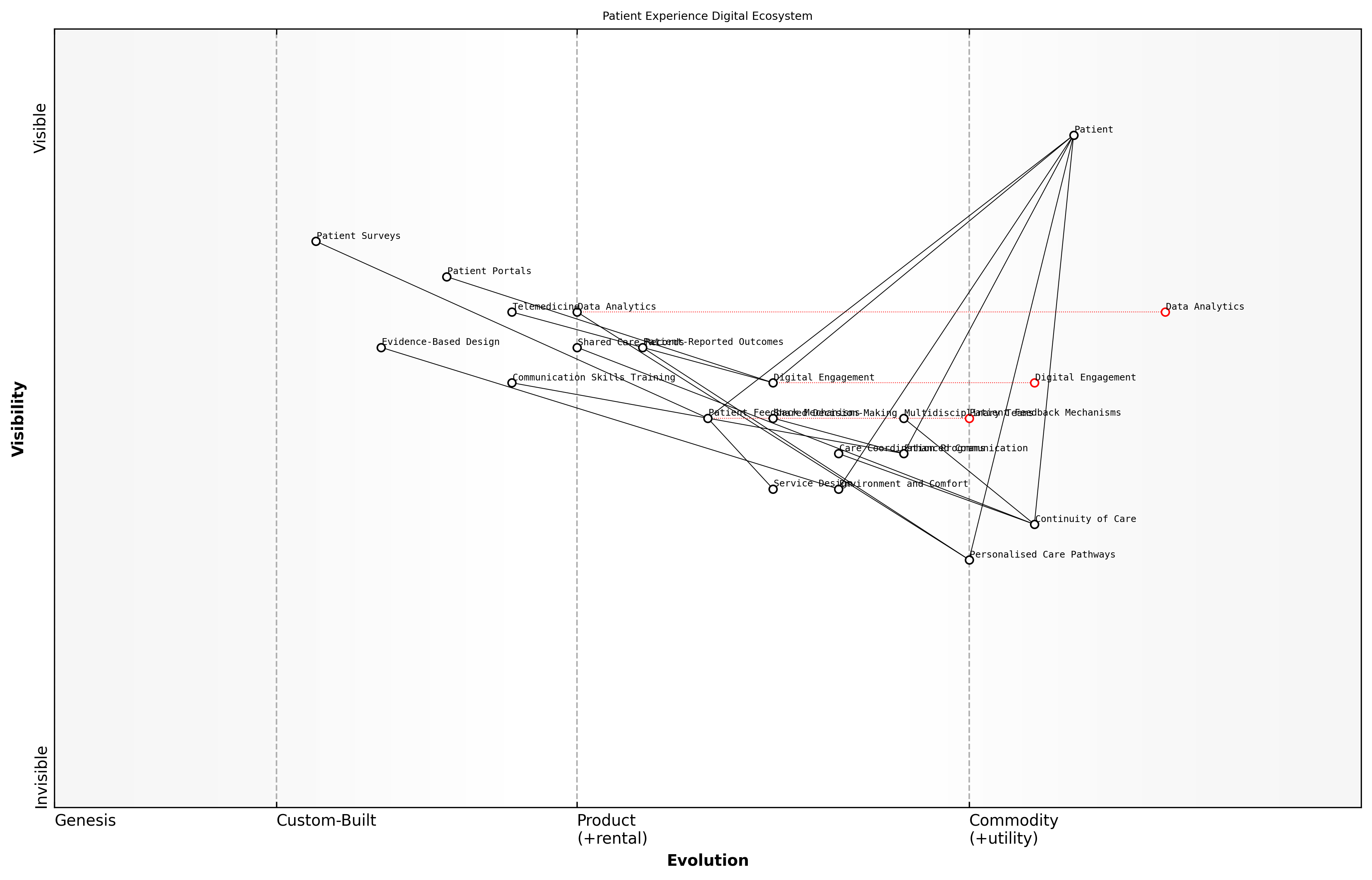
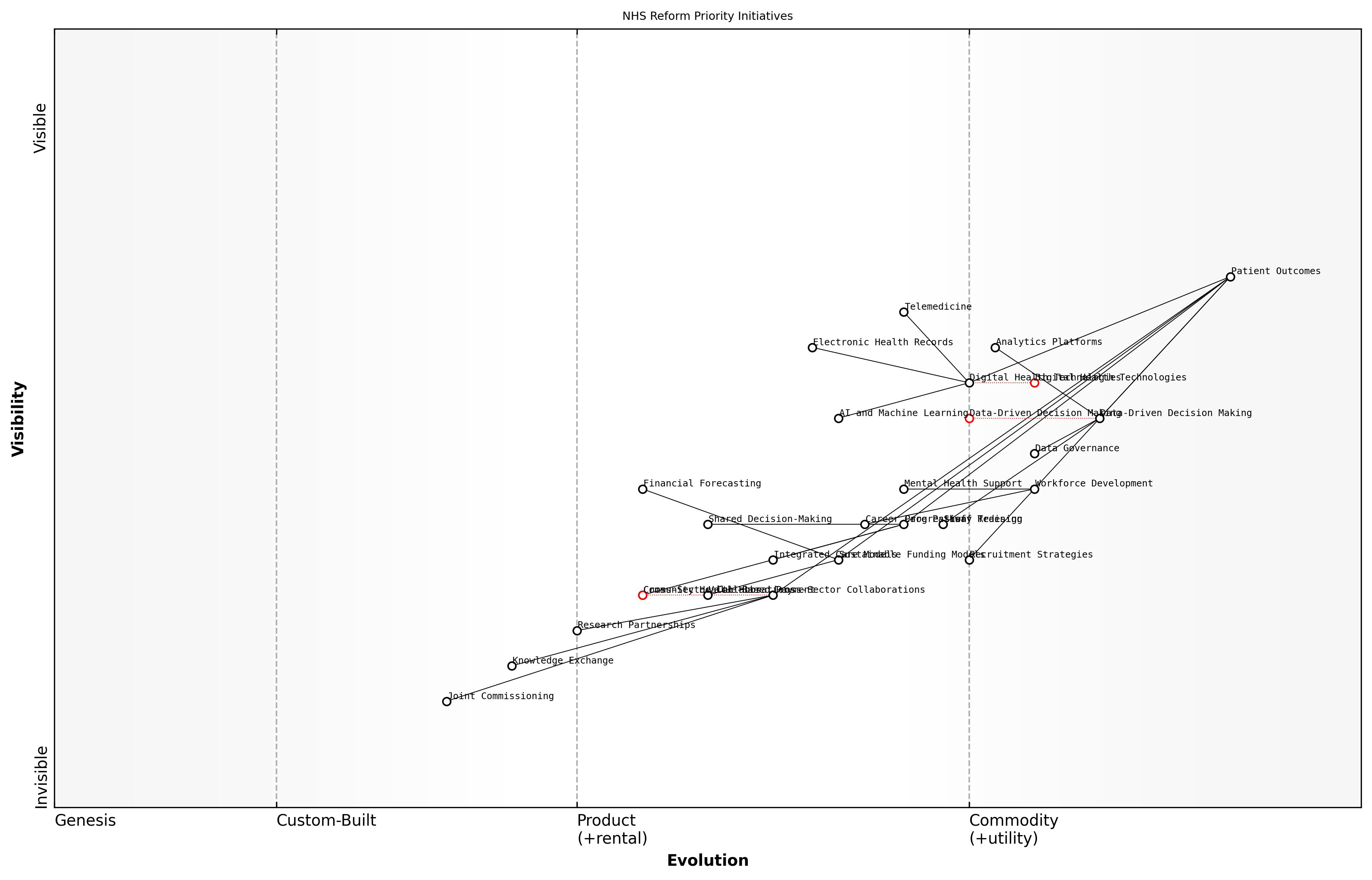
Wardley Map Assessment
The NHS Reform Strategy map presents a comprehensive approach to modernising and sustaining the NHS. It balances technological advancement with human-centred care, while addressing funding challenges and promoting collaboration. The strategy appears well-positioned to drive significant improvements, but success will depend on effective execution across all pillars, particularly in evolving areas like Cross-Sector Collaboration and Value-based Healthcare. Continuous reassessment and adaptation of the strategy will be crucial as the healthcare landscape evolves.
[View full Wardley Map report](markdown/wardley_map_reports/wardley_map_report_04_english_Key Areas for Reform.md)
These key areas for reform are not isolated initiatives but interconnected components of a comprehensive strategy to revitalise the NHS. Success in one area will invariably support and amplify efforts in others. For instance, effective digital transformation can enhance workforce efficiency, while patient-centred care models can contribute to more sustainable resource allocation by reducing unnecessary interventions.
The path to NHS reform is not about choosing between different priorities, but about orchestrating a symphony of changes that work in concert to create a healthcare system fit for the 21st century and beyond.
As we delve deeper into each of these reform areas in subsequent chapters, it is crucial to maintain a holistic perspective, understanding that true transformation of the NHS will require coordinated efforts across all these domains. The challenge ahead is significant, but by focusing on these key areas, we can chart a course towards a more resilient, efficient, and compassionate National Health Service that continues to embody the principles of universal healthcare while adapting to the evolving needs of the population it serves.
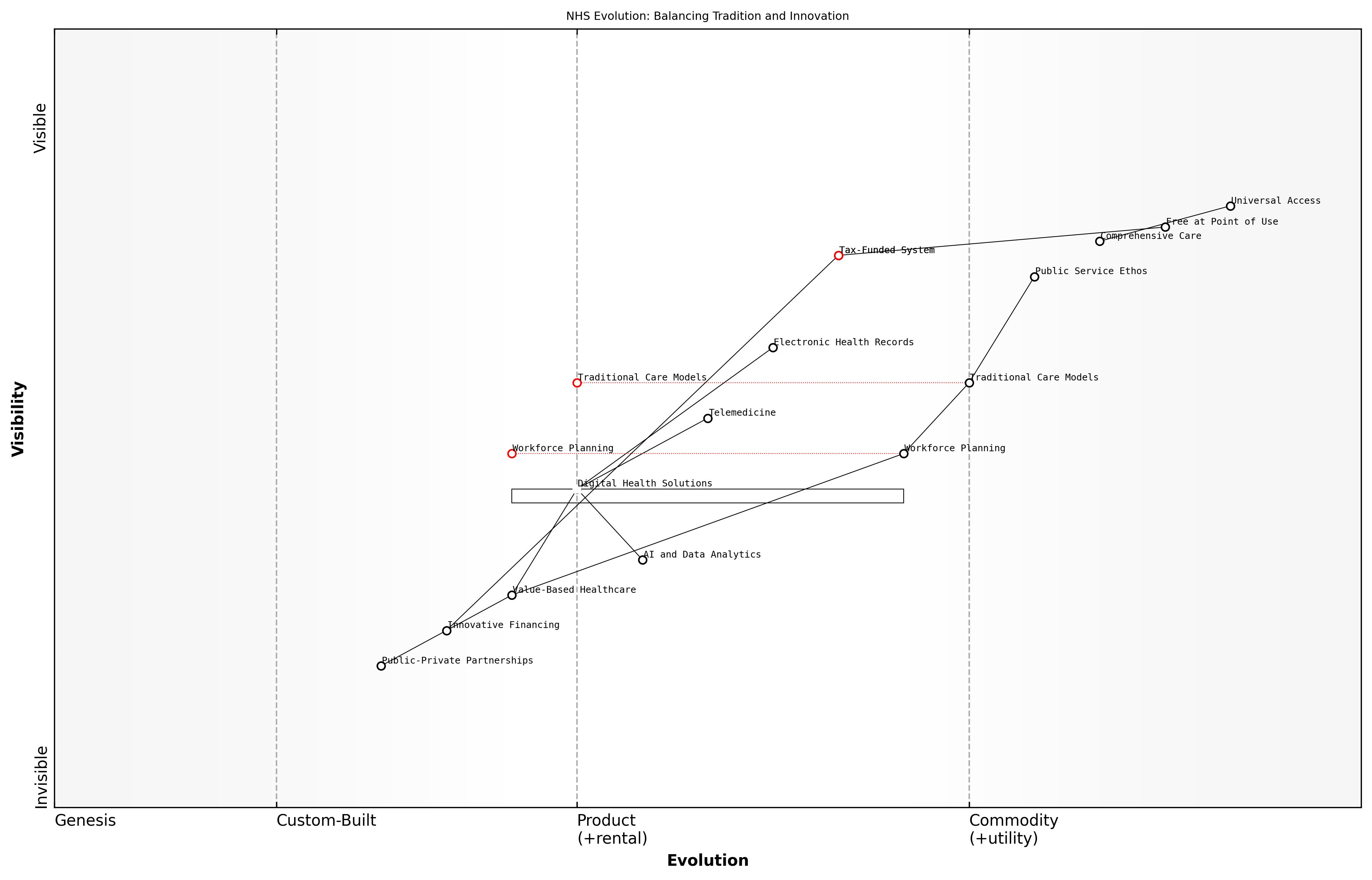
Balancing Tradition with Innovation
As we envision a revitalised NHS, one of the most critical challenges we face is striking the delicate balance between honouring the cherished traditions that have defined the service for decades and embracing the innovations necessary to meet the evolving healthcare needs of the 21st century. This balance is not merely a philosophical exercise; it is the cornerstone of a sustainable and effective healthcare system that can continue to deliver on its founding principles while adapting to new realities.
The NHS was built on noble principles: universal access, free at the point of use, and comprehensive care based on need rather than ability to pay. These principles have become deeply ingrained in the British social fabric and are a source of national pride. However, the healthcare landscape has changed dramatically since the NHS's inception in 1948. We now face an ageing population, a rise in chronic diseases, escalating costs of medical technologies, and increasing public expectations.
The NHS must evolve to meet the challenges of the 21st century while preserving the core values that have made it a beacon of healthcare equity worldwide.
Innovation in the NHS context does not mean wholesale abandonment of traditional practices. Rather, it involves a thoughtful integration of new technologies, care models, and organisational structures that can enhance and support the fundamental mission of the service. This approach requires a nuanced understanding of where tradition serves us well and where it may hinder progress.
- Preserving the ethos of universal access while implementing digital health solutions to improve accessibility
- Maintaining the personal touch in patient care while leveraging AI and data analytics for more precise diagnoses and treatments
- Upholding the principle of care based on need while introducing value-based healthcare models to ensure sustainability
- Retaining the NHS's role as a public service while exploring innovative public-private partnerships to drive efficiency and innovation
One area where this balance is particularly crucial is in the adoption of digital technologies. While telemedicine and electronic health records offer tremendous potential to improve efficiency and access to care, we must ensure that these innovations do not exacerbate existing health inequalities or depersonalise the care experience. This requires careful implementation strategies that consider the diverse needs of all patient populations.
Another key consideration is the workforce. The NHS has long been characterised by a culture of dedication and public service. As we introduce new ways of working and organisational structures, it's essential to preserve this ethos while also addressing longstanding issues such as burnout and staff shortages. This might involve innovative approaches to workforce planning, training, and support that respect the traditions of the profession while embracing new models of care delivery.
Innovation in the NHS should not be seen as a departure from its core values, but as a means to better fulfil its founding mission in a changing world.
Funding models present another area where tradition and innovation must be carefully balanced. While the principle of a tax-funded system remains popular and effective in many ways, we must explore innovative financing mechanisms to ensure long-term sustainability. This could involve new approaches to resource allocation, outcome-based commissioning, or social impact bonds, all while maintaining the fundamental principle of equitable access to care.
Ultimately, balancing tradition with innovation in the NHS requires a collaborative approach that engages all stakeholders – from policymakers and healthcare professionals to patients and the public. It demands clear communication about the rationale for change, transparency in decision-making processes, and a commitment to measuring and evaluating the impact of innovations on health outcomes and patient experience.
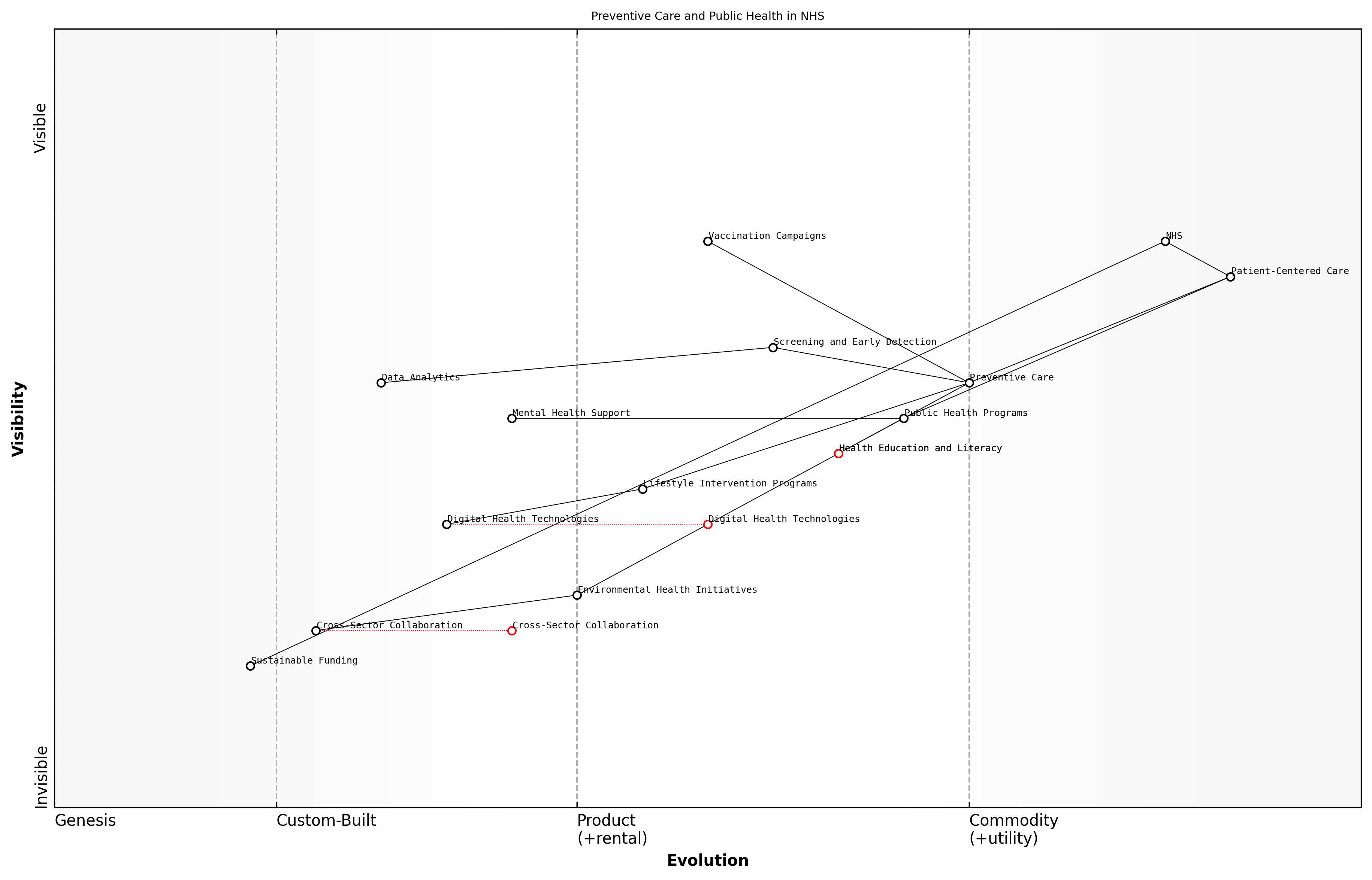
Wardley Map Assessment
The NHS is at a critical juncture, balancing its foundational principles with the need for innovation. By strategically integrating digital solutions and value-based approaches while maintaining its core ethos, the NHS can evolve to meet future healthcare challenges. Key focus areas should be workforce development, digital transformation, and innovative care models, all aligned with the overarching goal of improving patient outcomes while maintaining universal, free access to care.
[View full Wardley Map report](markdown/wardley_map_reports/wardley_map_report_05_english_Balancing Tradition with Innovation.md)
By carefully navigating this balance, we can create a vision for a revitalised NHS that honours its past while boldly facing the future. This approach will enable the service to continue its legacy of providing high-quality, equitable healthcare to all, adapting to new challenges while remaining true to the principles that have made it a national treasure. The path forward is not about choosing between tradition and innovation, but about harnessing the strengths of both to build a more resilient, effective, and compassionate healthcare system for generations to come.
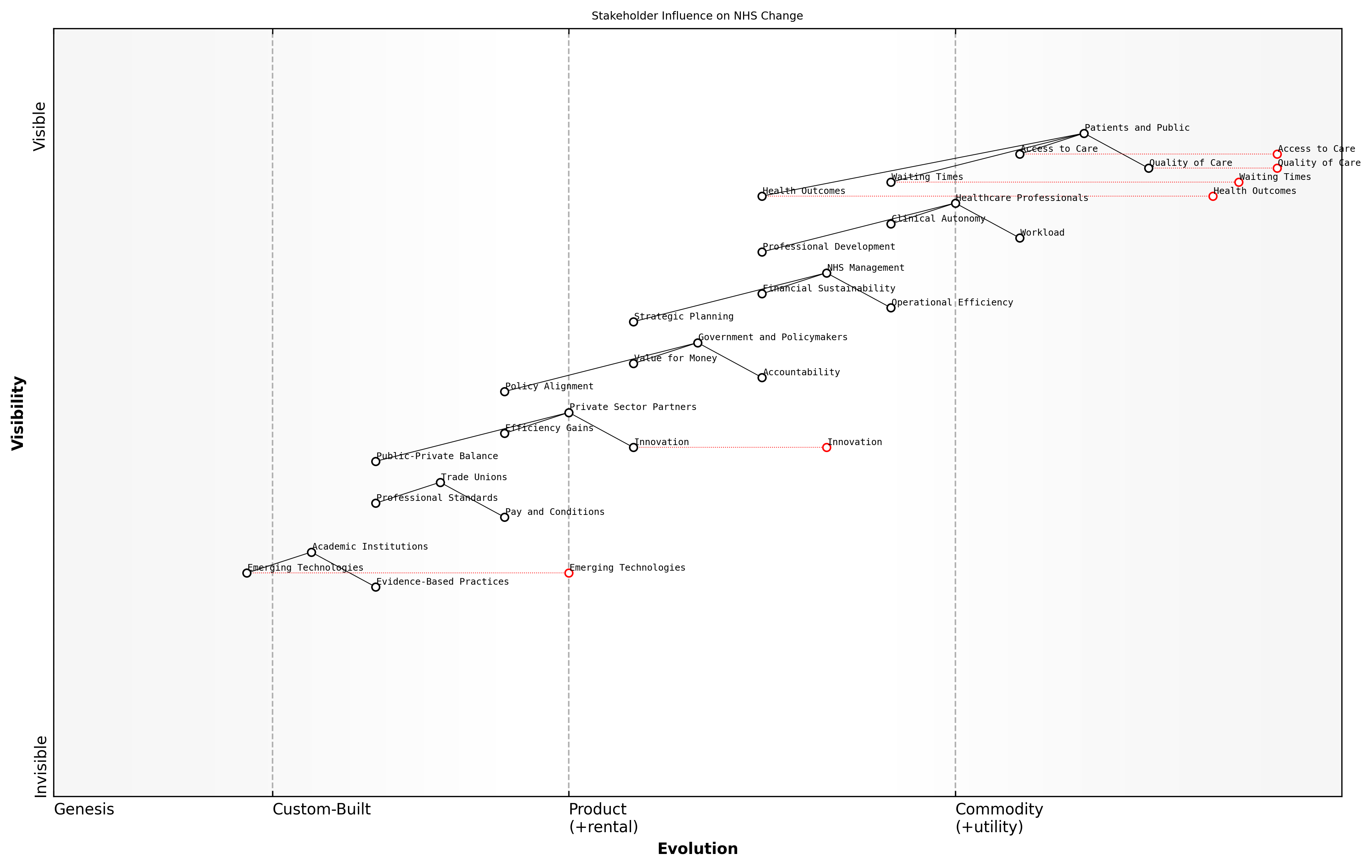
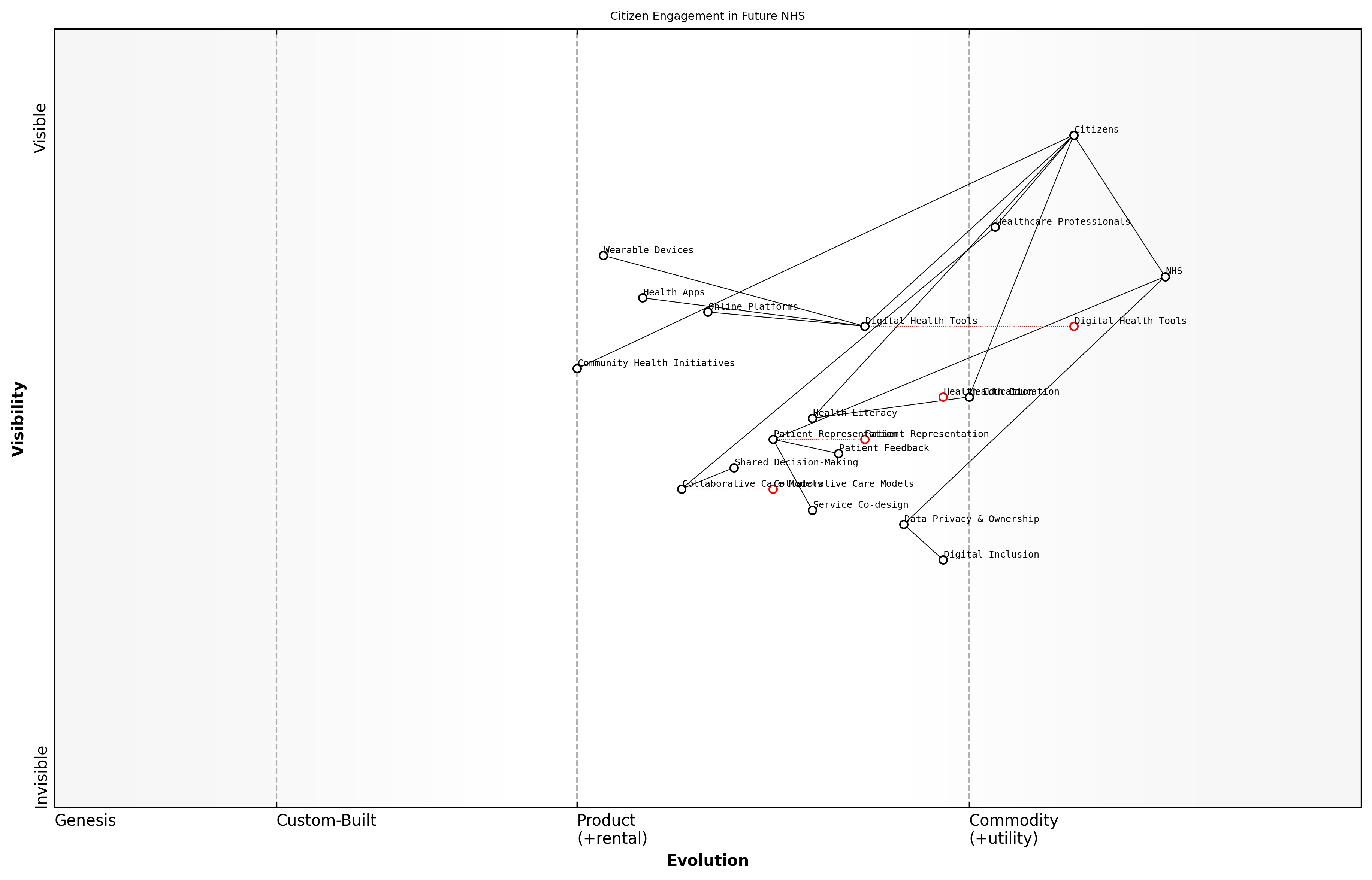
Stakeholder Perspectives on Change
As we envision a revitalised NHS, it is crucial to consider the diverse perspectives of key stakeholders who will both shape and be impacted by the transformation process. These stakeholders bring unique insights, concerns, and aspirations to the table, all of which must be carefully balanced to ensure a successful and sustainable reform of the healthcare system.
The complexity of the NHS ecosystem means that change will inevitably affect a wide range of groups, each with their own priorities and expectations. Understanding and addressing these varied perspectives is not just a matter of inclusivity; it is fundamental to the success of any large-scale reform initiative.
- Patients and the Public
- Healthcare Professionals
- NHS Management and Leadership
- Government and Policymakers
- Private Sector Partners
- Trade Unions and Professional Bodies
- Academic and Research Institutions
Patients and the public, as the end-users of the NHS, are primarily concerned with access to high-quality care, reduced waiting times, and improved health outcomes. Their perspective often focuses on the immediate and tangible aspects of healthcare delivery. A senior patient advocate aptly summarises this view:
What matters most to patients is not the intricacies of NHS structure, but whether they can see a doctor when they need to, receive effective treatment, and be treated with dignity and respect throughout their care journey.
Healthcare professionals, including doctors, nurses, and allied health workers, bring a frontline perspective to the change process. They are often enthusiastic about innovations that can improve patient care but may be wary of reforms that increase administrative burdens or threaten clinical autonomy. Their concerns typically revolve around workload, professional development, and the resources needed to deliver high-quality care.
NHS management and leadership teams are tasked with the complex challenge of balancing operational efficiency, financial sustainability, and quality of care. Their perspective often encompasses a broader view of system-wide challenges and the need for strategic, long-term solutions. As one NHS trust chief executive notes:
Our vision for change must be bold enough to address the fundamental challenges facing the NHS, yet practical enough to implement within the constraints of our current system. It's a delicate balance between ambition and realism.
Government and policymakers bring a national perspective, focusing on the broader health outcomes, economic implications, and political considerations of NHS reform. Their view often emphasises the need for accountability, value for money, and alignment with broader social and economic policies.
Private sector partners, including technology companies, pharmaceutical firms, and service providers, see opportunities for innovation and efficiency gains through increased collaboration with the NHS. However, their involvement often raises questions about the appropriate balance between public and private interests in healthcare delivery.
Trade unions and professional bodies play a crucial role in representing the interests of healthcare workers. Their perspective often focuses on workforce issues such as pay, working conditions, and professional standards. These organisations can be powerful allies in driving positive change but may also resist reforms perceived as threatening to their members' interests.
Academic and research institutions contribute valuable insights into evidence-based practices, emerging technologies, and global health trends. Their perspective often emphasises the importance of rigorous evaluation and continuous learning in driving healthcare improvements.
Balancing these diverse stakeholder perspectives is a formidable challenge, but it is essential for developing a vision of change that is both comprehensive and implementable. Successful NHS reform will require not only addressing the specific concerns of each group but also fostering a shared sense of purpose and collective responsibility for the future of healthcare in the UK.
Wardley Map Assessment
The Wardley Map reveals a complex, multi-stakeholder environment focused on improving patient outcomes while grappling with operational, financial, and political challenges. The NHS has significant strengths in its comprehensive coverage and clinical expertise, but faces challenges in areas such as digital transformation and sustainable financing. Strategic priorities should focus on leveraging technology and partnerships to enhance patient care, while addressing workforce concerns and operational efficiencies. The key to successful change will be in aligning the diverse stakeholder interests towards a common goal of a more effective, efficient, and patient-centric health service.
[View full Wardley Map report](markdown/wardley_map_reports/wardley_map_report_06_english_Stakeholder Perspectives on Change.md)
As we move forward with our vision for a revitalised NHS, it is crucial to create platforms for ongoing dialogue and collaboration among these diverse stakeholders. This approach will not only help in identifying potential synergies and conflicts but also in building the broad-based support necessary for implementing and sustaining transformative change in the NHS.
The path to a truly revitalised NHS lies not in imposing change from above, but in harnessing the collective wisdom, experience, and aspirations of all those who have a stake in its future. Only through genuine engagement and co-creation can we hope to build a healthcare system that is fit for the challenges of the 21st century.
Harnessing Data and Digital Technologies
Data-Driven Decision Making in Healthcare
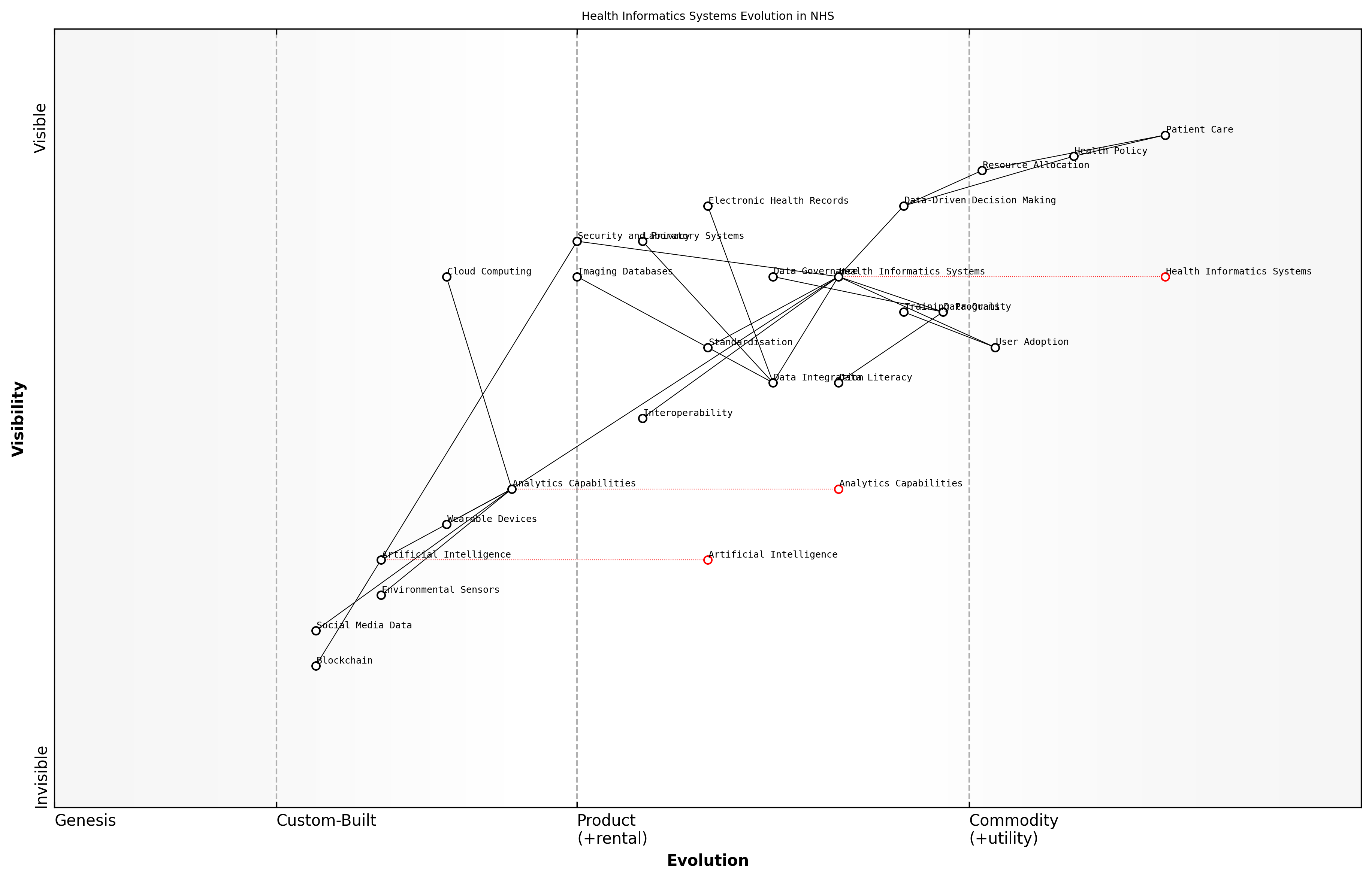
Building Robust Health Informatics Systems
In the realm of modern healthcare, robust health informatics systems serve as the backbone for data-driven decision making. These systems are essential for collecting, storing, analysing, and disseminating health-related information, enabling healthcare providers, policymakers, and researchers to make informed decisions that improve patient outcomes and optimise resource allocation within the NHS.
The development of robust health informatics systems requires a multifaceted approach that addresses technical, organisational, and ethical considerations. At its core, a robust system must ensure data accuracy, security, interoperability, and accessibility while adhering to stringent privacy regulations such as the General Data Protection Regulation (GDPR).
- Data Integration: Consolidating data from various sources, including electronic health records (EHRs), laboratory systems, and imaging databases
- Standardisation: Implementing uniform data standards and terminologies to ensure consistency across different healthcare settings
- Interoperability: Enabling seamless data exchange between different systems and healthcare providers
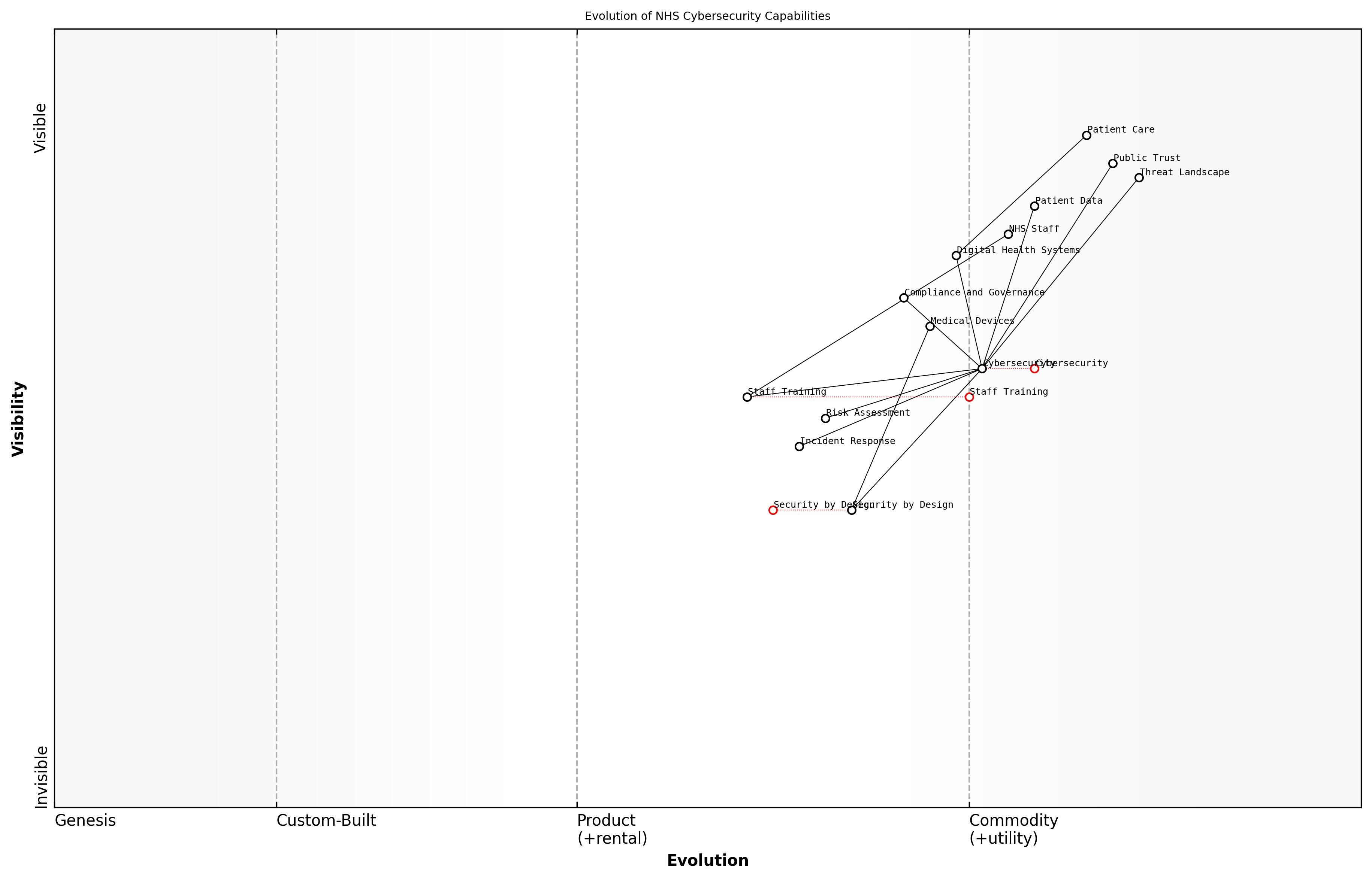
- Security and Privacy: Implementing robust cybersecurity measures and ensuring compliance with data protection regulations
- Analytics Capabilities: Incorporating advanced analytics tools for data mining, predictive modelling, and real-time reporting
One of the key challenges in building robust health informatics systems within the NHS is the legacy of disparate, siloed systems that have evolved over time. Overcoming this challenge requires a strategic approach to system integration and data harmonisation. This involves not only technical solutions but also organisational change management to ensure that healthcare professionals are equipped to effectively utilise these systems in their daily practice.
The future of healthcare lies in our ability to harness the power of data. Robust health informatics systems are not just a technological upgrade; they are a fundamental shift in how we approach patient care, resource allocation, and health policy decision-making.
To build truly robust health informatics systems, the NHS must invest in cutting-edge technologies such as cloud computing, artificial intelligence, and blockchain. Cloud computing offers scalability and flexibility, allowing health systems to manage large volumes of data efficiently. Artificial intelligence can be leveraged for advanced analytics, pattern recognition, and decision support. Blockchain technology holds promise for enhancing data security and enabling secure, decentralised data sharing across the healthcare ecosystem.
However, technology alone is not sufficient. The success of health informatics systems depends heavily on user adoption and data quality. Therefore, comprehensive training programmes for healthcare professionals, coupled with initiatives to improve data literacy across the NHS workforce, are crucial. Additionally, establishing clear governance structures and data quality assurance processes is essential to maintain the integrity and reliability of the information within these systems.
- Implement continuous data quality monitoring and improvement processes
- Develop user-friendly interfaces that align with clinical workflows
- Establish clear data governance policies and accountability measures
- Invest in ongoing training and support for system users
- Foster a culture of data-driven decision making across all levels of the NHS
The implementation of robust health informatics systems also presents an opportunity to address health inequalities. By capturing and analysing comprehensive data on population health, social determinants, and healthcare utilisation patterns, the NHS can identify underserved populations and tailor interventions to address specific health needs. This data-driven approach to health equity aligns with the NHS's core principle of providing universal access to healthcare.
In the digital age, health informatics is not just about technology; it's about transforming raw data into actionable insights that can save lives, improve health outcomes, and ensure the efficient use of our limited healthcare resources.
As we look to the future, the potential of robust health informatics systems extends beyond traditional healthcare settings. The integration of data from wearable devices, environmental sensors, and social media platforms offers new avenues for population health management and personalised medicine. However, this also raises new ethical considerations regarding data ownership, consent, and the responsible use of personal health information.
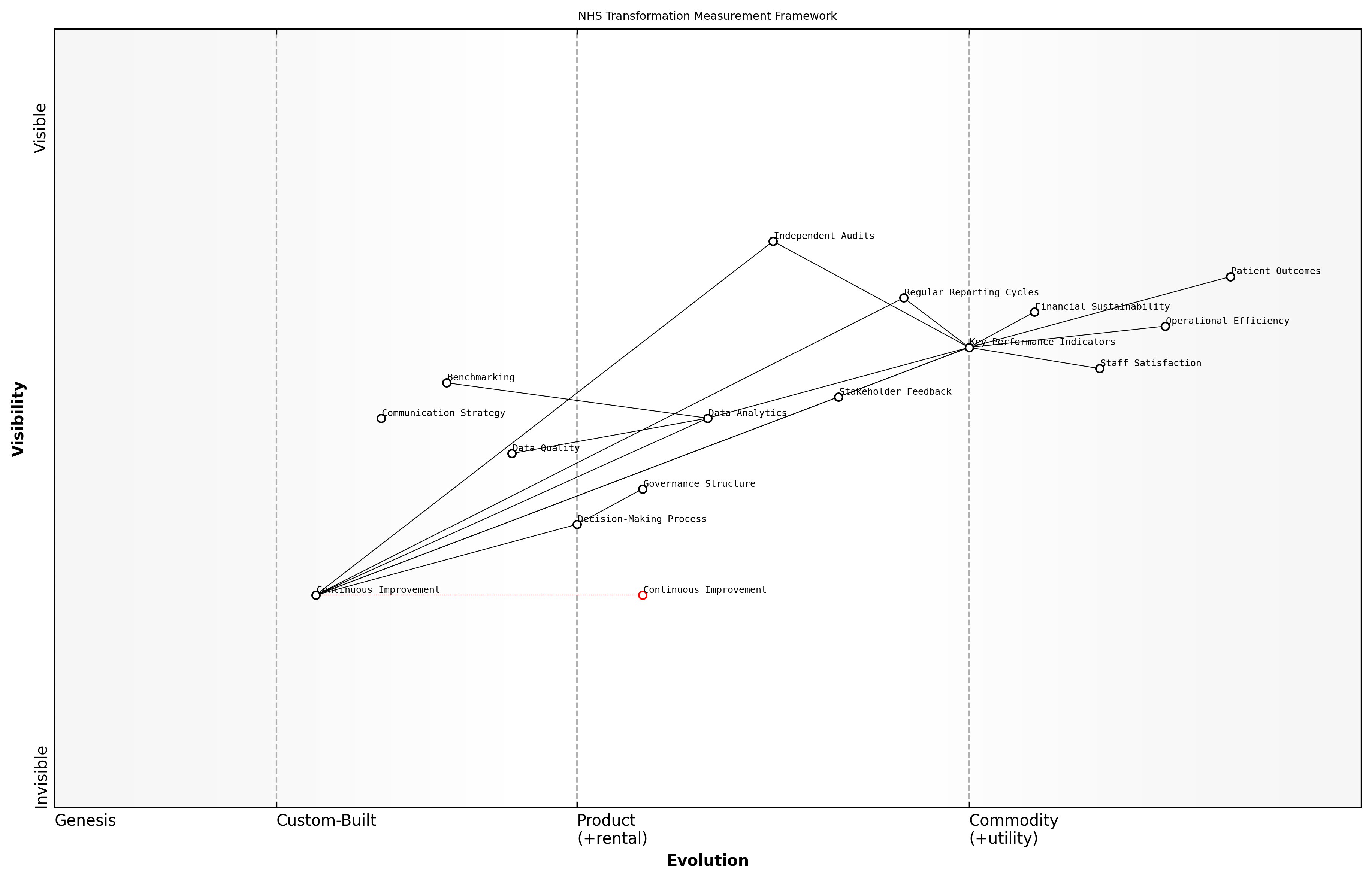
Wardley Map Assessment
The NHS is on the right track with its focus on data-driven decision making and robust health informatics systems. However, to maintain its position and improve patient care, it needs to accelerate the evolution of key components, particularly in AI, data integration, and user adoption. By addressing these areas and leveraging emerging technologies, the NHS can create a more efficient, effective, and future-proof healthcare system.
[View full Wardley Map report](markdown/wardley_map_reports/wardley_map_report_07_english_Building Robust Health Informatics Systems.md)
In conclusion, building robust health informatics systems is a critical step in transforming the NHS for the digital age. It requires a holistic approach that combines technological innovation with organisational change, ethical considerations, and a commitment to data-driven decision making. By investing in these systems, the NHS can enhance its ability to deliver high-quality, efficient, and equitable healthcare services to all citizens, ultimately fulfilling its mission of providing comprehensive health coverage in an increasingly complex and data-rich world.
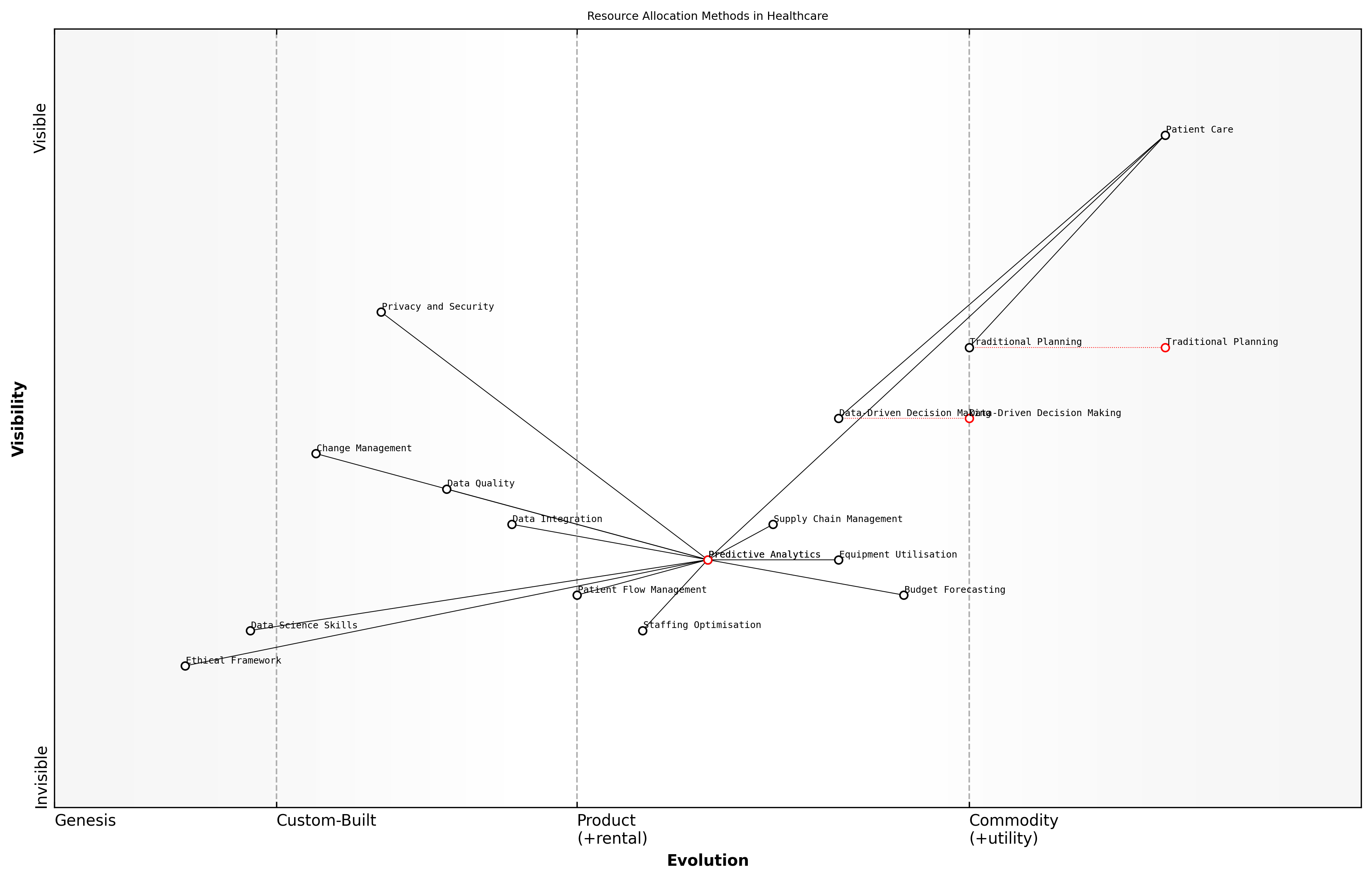
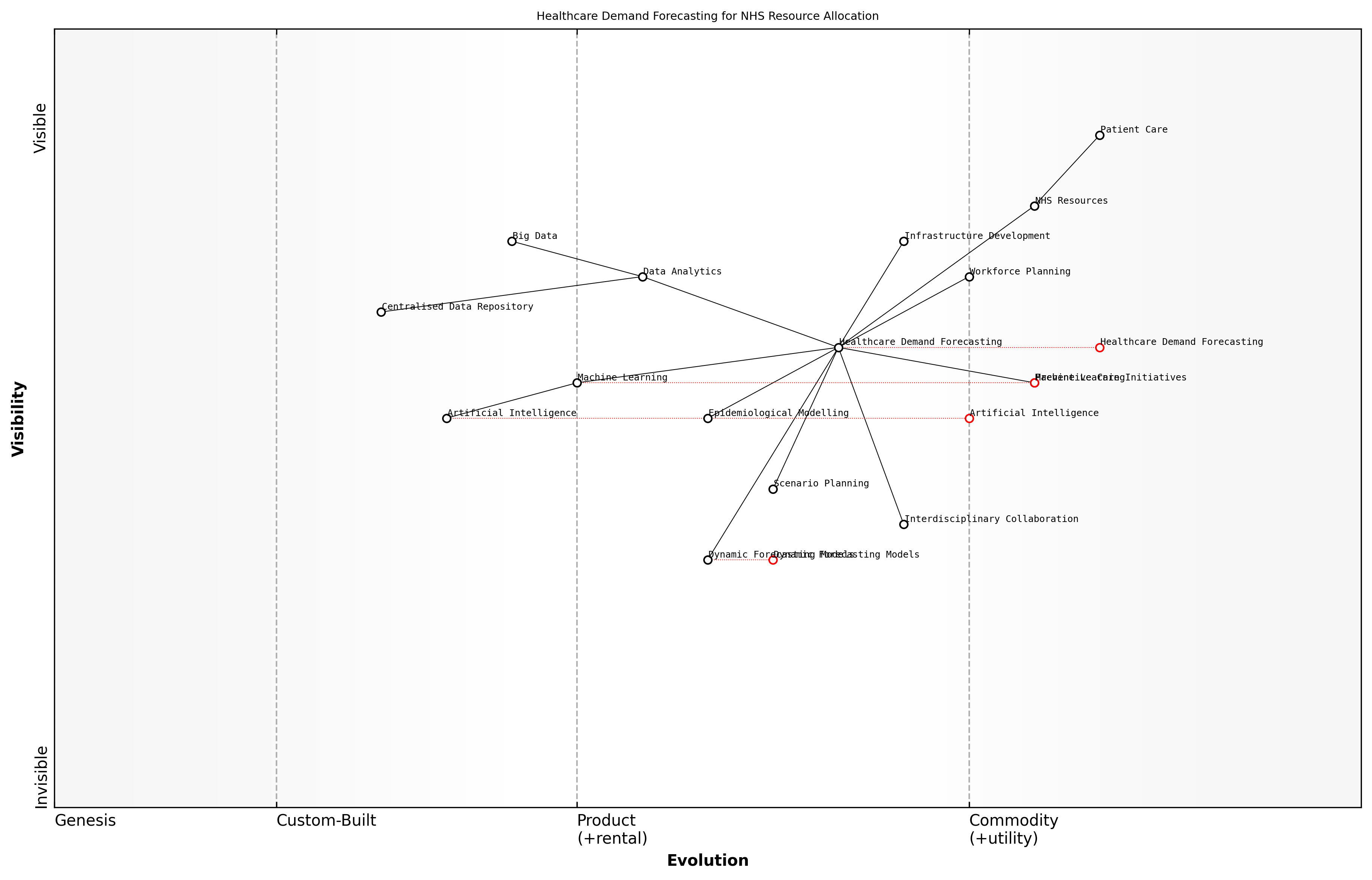
Predictive Analytics for Resource Allocation
In the realm of data-driven decision making in healthcare, predictive analytics for resource allocation stands out as a transformative approach that can significantly enhance the efficiency and effectiveness of the NHS. As an expert who has advised numerous healthcare organisations on implementing advanced analytics solutions, I can attest to the profound impact this technology can have on optimising resource utilisation and improving patient outcomes.
Predictive analytics in healthcare involves using historical data, statistical algorithms, and machine learning techniques to identify the likelihood of future outcomes. When applied to resource allocation within the NHS, it can revolutionise how we manage everything from staffing levels to medical supplies and equipment distribution.
Predictive analytics is not just about forecasting; it's about creating a proactive healthcare system that anticipates needs and allocates resources with unprecedented precision.
The implementation of predictive analytics for resource allocation in the NHS can be broken down into several key areas:
- Patient Flow Management
- Staffing Optimisation
- Supply Chain Management
- Equipment Utilisation
- Budget Forecasting
Patient Flow Management: By analysing historical patient data, seasonal trends, and local demographics, predictive models can forecast patient admissions, length of stay, and discharge rates. This information is crucial for optimising bed allocation, reducing wait times, and ensuring that resources are available where and when they are needed most.
Staffing Optimisation: Predictive analytics can help NHS trusts anticipate staffing needs based on expected patient volumes and acuity levels. This enables more efficient scheduling, reduces overtime costs, and ensures appropriate staff-to-patient ratios, ultimately improving both patient care and staff satisfaction.
Supply Chain Management: By predicting demand for medical supplies, pharmaceuticals, and other consumables, the NHS can optimise its supply chain, reduce waste, and ensure critical resources are always available. This is particularly crucial in times of crisis, such as during pandemics or natural disasters.
Equipment Utilisation: Predictive models can forecast the need for medical equipment, from MRI machines to ventilators, allowing for more efficient scheduling and maintenance. This not only improves patient access to diagnostic and treatment tools but also extends the lifespan of expensive medical equipment.
Budget Forecasting: By analysing historical spending patterns and predicting future resource needs, predictive analytics can help NHS trusts and Clinical Commissioning Groups (CCGs) create more accurate budgets and allocate funds more effectively across different departments and services.
The power of predictive analytics lies in its ability to turn vast amounts of healthcare data into actionable insights that drive smarter, more proactive decision-making.
However, implementing predictive analytics for resource allocation in the NHS is not without its challenges. These include:
- Data Quality and Integration
- Privacy and Security Concerns
- Resistance to Change
- Skill Gap in Data Science
- Ethical Considerations
Data Quality and Integration: The NHS, like many large healthcare systems, often struggles with data silos and inconsistent data quality across different trusts and departments. Ensuring clean, integrated data is crucial for accurate predictive modelling.
Privacy and Security Concerns: The sensitive nature of healthcare data means that robust security measures and strict adherence to data protection regulations like GDPR are essential when implementing predictive analytics systems.
Resistance to Change: Healthcare professionals may be hesitant to trust algorithmic predictions over their clinical judgement. Overcoming this resistance requires clear communication, training, and demonstrable benefits of the predictive models.
Skill Gap in Data Science: There is a shortage of data scientists and analysts with healthcare domain knowledge. The NHS must invest in training existing staff and recruiting specialists to fully leverage predictive analytics capabilities.
Ethical Considerations: Predictive models must be carefully designed and monitored to avoid perpetuating biases or exacerbating health inequalities. Ethical frameworks for the use of AI and predictive analytics in healthcare decision-making are crucial.
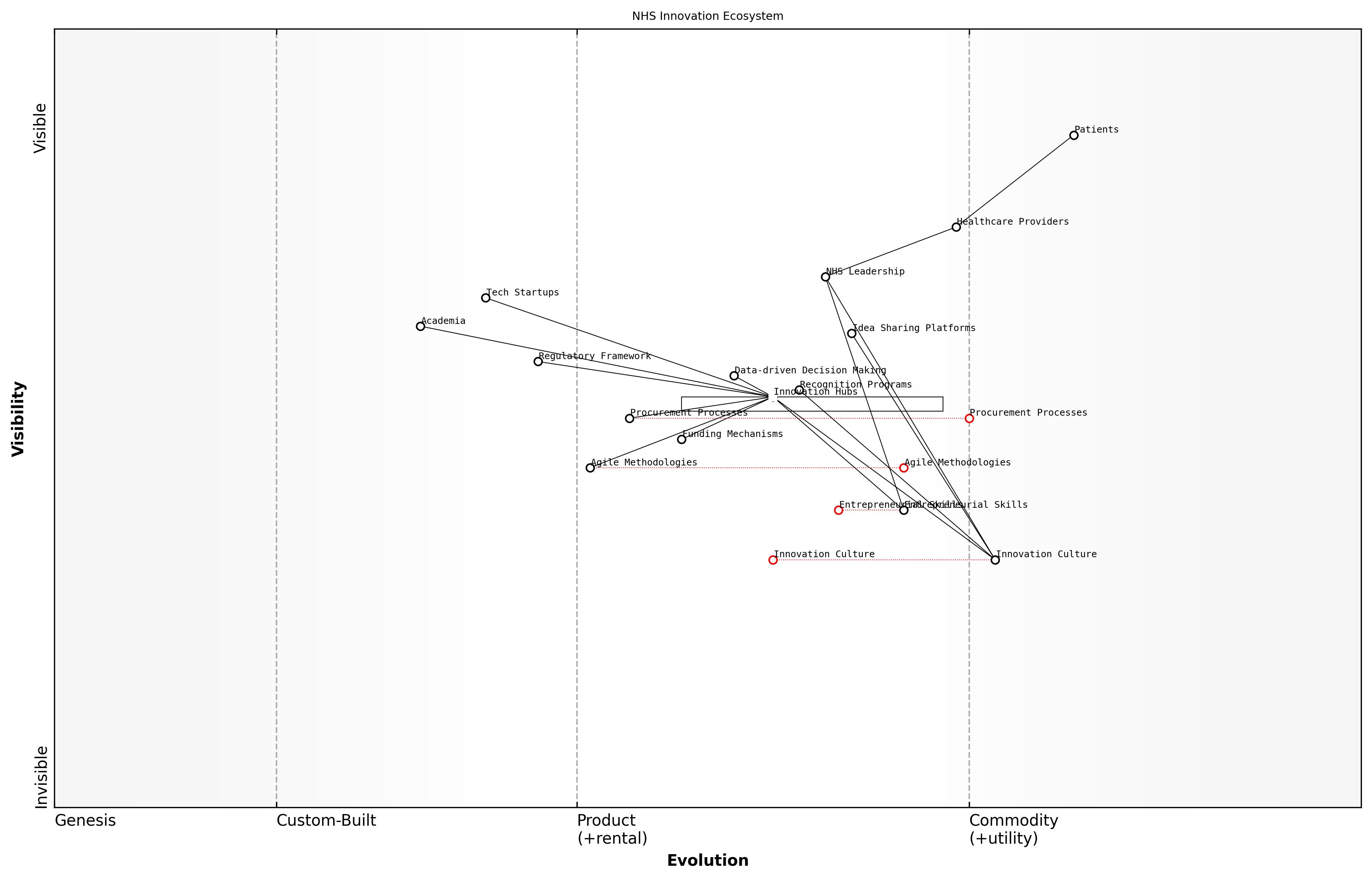
Wardley Map Assessment
This Wardley Map reveals a healthcare system in transition, moving from traditional resource allocation methods to more sophisticated, data-driven approaches. The strategic focus should be on developing predictive analytics capabilities while simultaneously addressing ethical considerations and data science skill gaps. Success will depend on balancing technological advancement with patient-centric care and ethical responsibility.
[View full Wardley Map report](markdown/wardley_map_reports/wardley_map_report_08_english_Predictive Analytics for Resource Allocation.md)
Despite these challenges, the potential benefits of predictive analytics for resource allocation in the NHS are immense. By enabling more efficient use of limited resources, predictive analytics can help the NHS deliver better care to more patients while controlling costs. As we look to the future of healthcare in the UK, the integration of predictive analytics into resource allocation strategies will be a key factor in creating a more responsive, efficient, and sustainable NHS.
The successful implementation of predictive analytics for resource allocation represents a significant step towards a truly data-driven NHS, capable of meeting the healthcare challenges of the 21st century.
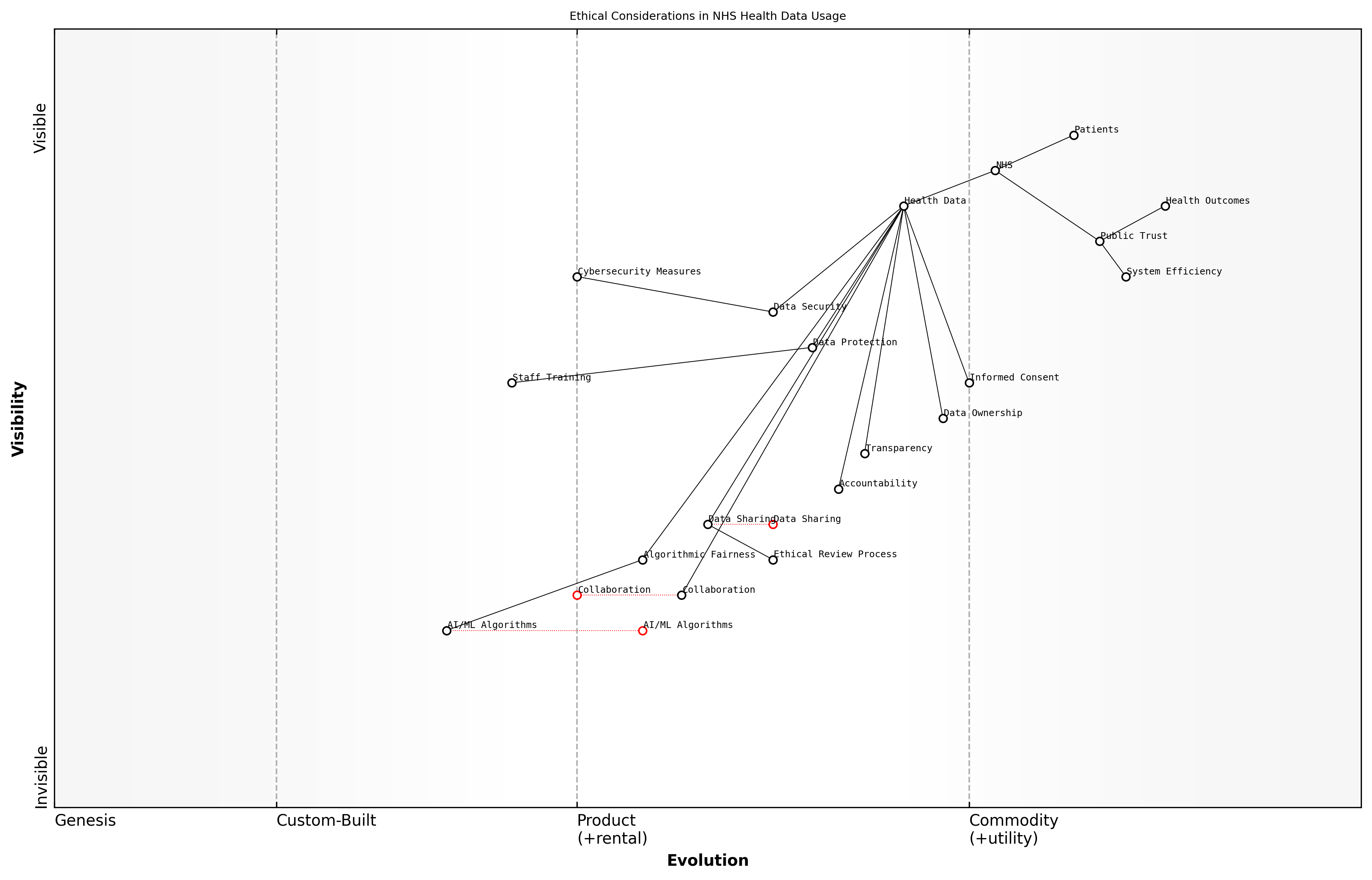
Ethical Considerations in Health Data Usage
As we delve deeper into the realm of data-driven decision making in healthcare, it is imperative that we address the ethical considerations surrounding health data usage. The NHS, as a public institution entrusted with the care and well-being of millions, must navigate this complex landscape with utmost diligence and responsibility. The potential benefits of leveraging vast amounts of health data are immense, but so too are the risks if not managed properly.
At the heart of this issue lies the tension between the collective good that can be achieved through comprehensive data analysis and the individual right to privacy and data protection. The NHS must strike a delicate balance, ensuring that the wealth of data at its disposal is used to improve patient outcomes and system efficiency, while simultaneously safeguarding the confidentiality and autonomy of each patient.
- Informed Consent and Data Ownership
- Data Security and Protection
- Algorithmic Bias and Fairness
- Transparency and Accountability
- Data Sharing and Collaboration
Informed consent is a cornerstone of ethical health data usage. Patients must be fully aware of how their data will be used, who will have access to it, and for what purposes. This extends beyond the traditional doctor-patient relationship to include the myriad ways in which data can be analysed and applied in modern healthcare systems. The NHS must develop clear, accessible frameworks for obtaining and managing patient consent, ensuring that individuals retain control over their personal health information.
The future of healthcare lies in our ability to harness the power of data while maintaining the trust of those we serve. Without this trust, the potential of data-driven decision making will remain unfulfilled.
Data security and protection are paramount in maintaining this trust. The NHS must invest in robust cybersecurity measures and data governance frameworks to prevent unauthorised access, breaches, and misuse of sensitive health information. This includes not only technical solutions but also comprehensive staff training and the cultivation of a culture that prioritises data protection at all levels of the organisation.
As we increasingly rely on artificial intelligence and machine learning algorithms to analyse health data and inform decision-making, we must be vigilant about the potential for algorithmic bias. These systems can inadvertently perpetuate or even exacerbate existing health inequalities if not carefully designed and monitored. The NHS must prioritise the development of fair, transparent algorithms that account for the diverse population it serves.
Transparency and accountability are crucial in maintaining public trust in the NHS's data practices. Clear communication about how data is being used, regular audits of data systems and practices, and mechanisms for addressing concerns and complaints should be established. This openness will not only build trust but also foster a collaborative approach to improving data usage practices over time.
The potential for data sharing and collaboration in healthcare is immense, offering opportunities for groundbreaking research and improved patient care. However, the NHS must navigate the ethical complexities of sharing sensitive health data with other organisations, be they academic institutions, private companies, or other healthcare providers. Robust frameworks for data sharing agreements, anonymisation techniques, and ethical review processes must be put in place to ensure that collaborative efforts do not compromise patient privacy or trust.
In the age of big data, our ethical frameworks must evolve as rapidly as our technological capabilities. We have a responsibility to ensure that every byte of data we collect serves to improve health outcomes while respecting individual rights and societal values.
As we move forward with data-driven decision making in the NHS, it is crucial that ethical considerations are not treated as an afterthought but are instead woven into the very fabric of our data strategies and practices. By doing so, we can harness the full potential of health data to transform patient care, improve system efficiency, and address health inequalities, all while maintaining the trust and confidence of the public we serve.
Wardley Map Assessment
The NHS is in a strong position to leverage its comprehensive health data and public trust to drive innovations in healthcare delivery. However, it must carefully navigate the ethical challenges posed by emerging technologies and data sharing practices. By focusing on strengthening its ethical frameworks, enhancing data security, and fostering a culture of responsible innovation, the NHS can maintain its position as a leader in ethical, data-driven healthcare. The key to success lies in balancing rapid technological advancement with robust ethical considerations and unwavering commitment to patient trust and well-being.
[View full Wardley Map report](markdown/wardley_map_reports/wardley_map_report_09_english_Ethical Considerations in Health Data Usage.md)
Digital Transformation Strategies
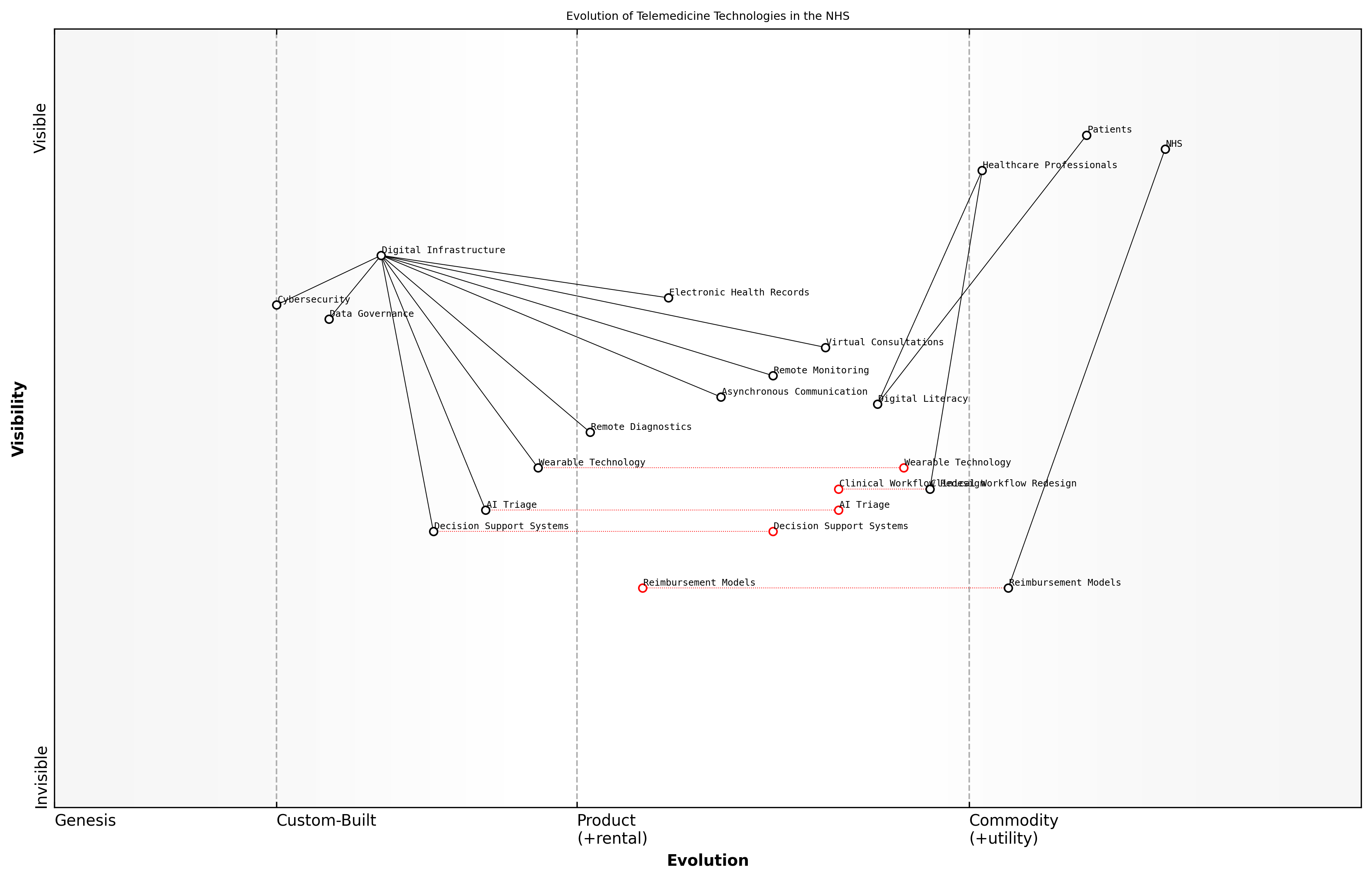
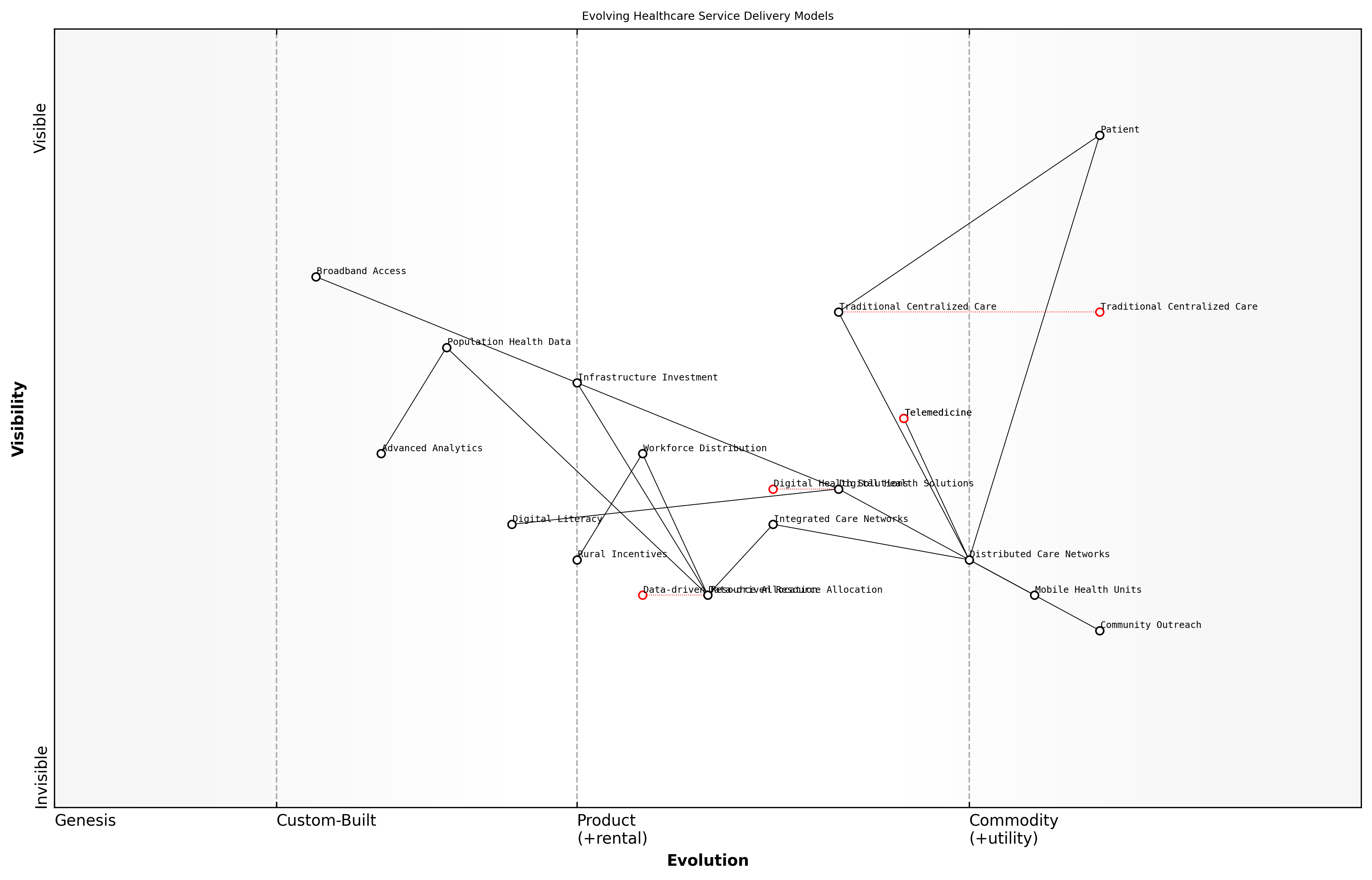
Telemedicine and Remote Care Solutions
Telemedicine and remote care solutions represent a transformative shift in healthcare delivery, offering unprecedented opportunities to enhance access, improve patient outcomes, and optimise resource allocation within the NHS. As we navigate the complexities of modernising our healthcare system, these digital innovations stand at the forefront of our strategy to create a more resilient, efficient, and patient-centric NHS.
The COVID-19 pandemic has accelerated the adoption of telemedicine, demonstrating its potential to revolutionise healthcare delivery. However, to fully harness its benefits, we must approach implementation strategically, addressing both technological and human factors.
- Virtual consultations and remote monitoring
- Asynchronous communication platforms
- Integration with electronic health records
- AI-powered triage and decision support systems
- Remote diagnostics and wearable technology
Virtual consultations and remote monitoring form the backbone of telemedicine, allowing healthcare professionals to assess, diagnose, and treat patients without the need for in-person visits. This not only improves access for patients in rural or underserved areas but also reduces the strain on physical NHS facilities. Asynchronous communication platforms, such as secure messaging systems, enable efficient follow-ups and routine care management, freeing up valuable clinical time for more complex cases.
Telemedicine isn't just about replicating in-person care through a screen; it's about reimagining healthcare delivery to be more accessible, efficient, and patient-centred.
The integration of telemedicine solutions with electronic health records (EHRs) is crucial for ensuring continuity of care and enabling data-driven decision-making. By seamlessly incorporating remote care data into patients' comprehensive health records, we can facilitate more informed clinical decisions and improve care coordination across different healthcare settings.
AI-powered triage and decision support systems represent the next frontier in telemedicine. These technologies can analyse patient symptoms, medical history, and real-time data to prioritise cases, suggest appropriate care pathways, and even assist in diagnosis. While not replacing clinical judgement, these tools can significantly enhance efficiency and accuracy in remote care settings.
Remote diagnostics and wearable technology are rapidly expanding the capabilities of telemedicine. From smartphone-based ECG monitors to continuous glucose sensors, these devices allow for real-time monitoring of patient health metrics, enabling proactive interventions and personalised care plans. The NHS must strategically invest in and integrate these technologies to fully realise their potential in improving patient outcomes and reducing hospital readmissions.
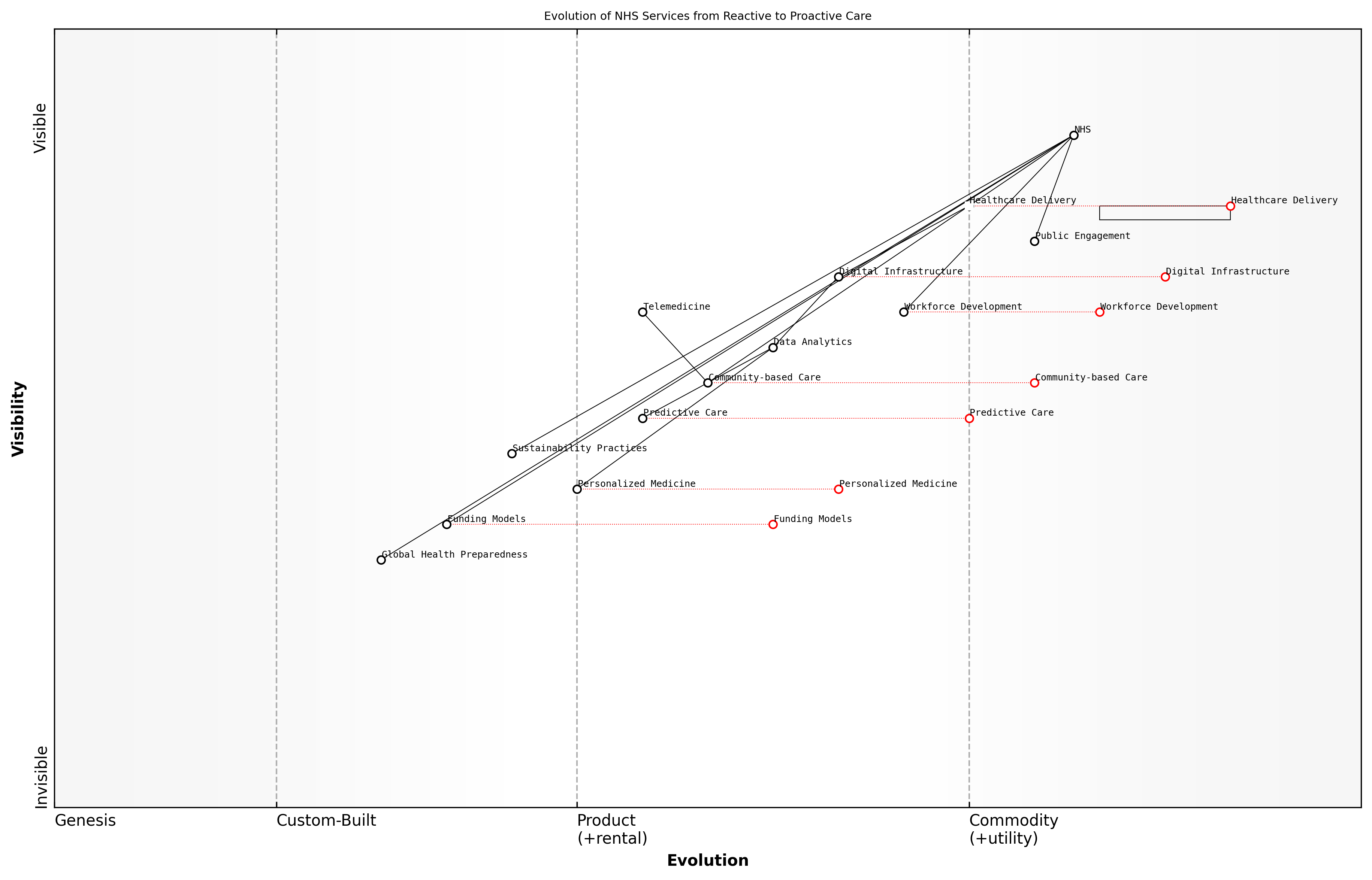
Wardley Map Assessment
The NHS is progressing well in its telemedicine evolution but faces challenges in rapidly advancing technologies and organisational adaptations. Key focus areas should be accelerating AI integration, enhancing digital literacy, and evolving reimbursement models to support new care delivery methods. The strong foundation in digital infrastructure and electronic health records provides a solid base for future innovations. Success will depend on balancing technological advancements with workforce development and organisational change management.
[View full Wardley Map report](markdown/wardley_map_reports/wardley_map_report_10_english_Telemedicine and Remote Care Solutions.md)
However, the successful implementation of telemedicine and remote care solutions within the NHS faces several challenges that must be addressed:
- Ensuring equitable access to technology and digital literacy
- Maintaining data privacy and cybersecurity
- Adapting clinical workflows and training healthcare professionals
- Developing appropriate reimbursement models for remote care
- Addressing the potential for increased health inequalities
To overcome these challenges, a multi-faceted approach is required. This includes investing in digital infrastructure, particularly in underserved areas, and providing digital literacy support for both patients and healthcare professionals. Robust data governance frameworks and cybersecurity measures must be implemented to protect patient information and maintain trust in telemedicine systems.
Clinical workflows must be redesigned to effectively incorporate remote care, supported by comprehensive training programmes for healthcare staff. This cultural shift towards digital-first care delivery is essential for the long-term success of telemedicine initiatives within the NHS.
The true measure of success for telemedicine in the NHS will be its ability to seamlessly integrate with traditional care models, enhancing rather than replacing the human touch in healthcare.
Reimbursement models for telemedicine services need careful consideration to ensure they incentivise appropriate use of remote care while maintaining financial sustainability. This may involve a combination of fee-for-service and value-based payment models tailored to the unique aspects of telemedicine delivery.
Finally, it is crucial to monitor and address any potential exacerbation of health inequalities resulting from the shift to digital care. This includes ensuring that telemedicine complements rather than replaces in-person care options, particularly for vulnerable populations who may face barriers to digital access.
By thoughtfully implementing telemedicine and remote care solutions, the NHS can significantly enhance its capacity to deliver high-quality, accessible healthcare. These digital transformation strategies, when properly executed, have the potential to create a more resilient, efficient, and patient-centred health service, capable of meeting the evolving needs of the UK population in the 21st century.
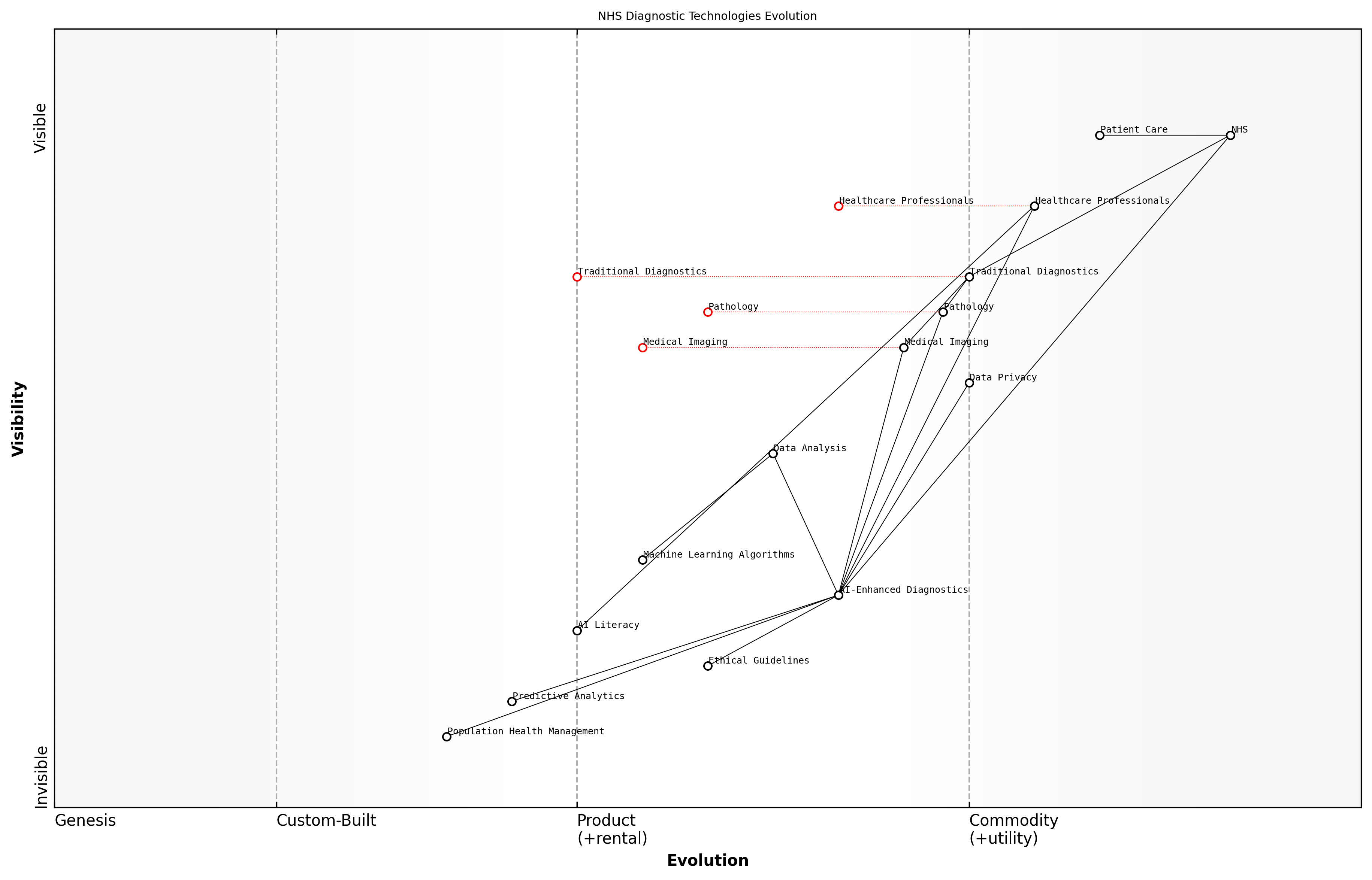
AI and Machine Learning in Diagnostics
Artificial Intelligence (AI) and Machine Learning (ML) are revolutionising diagnostic processes within the NHS, offering unprecedented opportunities to enhance accuracy, speed, and efficiency in patient care. As we navigate the complex landscape of digital transformation in healthcare, these technologies stand at the forefront of innovation, promising to alleviate pressure on overstretched resources and improve patient outcomes.
The integration of AI and ML into diagnostic procedures represents a paradigm shift in how we approach healthcare delivery. These technologies have the potential to analyse vast amounts of medical data, including imaging studies, pathology reports, and patient histories, at a speed and level of detail that surpasses human capabilities. This not only accelerates the diagnostic process but also enhances its precision, potentially leading to earlier detection of diseases and more personalised treatment plans.
AI and machine learning are not just tools; they are catalysts for a new era of precision medicine within the NHS. By harnessing these technologies, we can unlock insights from complex medical data that were previously beyond our reach, leading to more accurate diagnoses and tailored treatments.
One of the most promising applications of AI in diagnostics is in medical imaging. Advanced algorithms can now analyse radiological images such as X-rays, MRIs, and CT scans with remarkable accuracy. These AI systems can detect subtle abnormalities that might be overlooked by even the most experienced radiologists, serving as a powerful second opinion and reducing the risk of misdiagnosis. Moreover, they can prioritise urgent cases, ensuring that critical conditions receive immediate attention, thus potentially saving lives in time-sensitive situations.
- Enhanced accuracy in image interpretation, reducing human error
- Faster analysis of medical images, leading to quicker diagnoses
- Prioritisation of urgent cases, improving emergency response times
- Detection of subtle patterns and anomalies that human observers might miss
- Standardisation of diagnostic processes across different NHS trusts
In pathology, AI and ML algorithms are being employed to analyse tissue samples and blood tests with unprecedented precision. These systems can identify cellular abnormalities, predict disease progression, and even suggest the most effective treatment options based on genetic markers. This level of analysis not only improves diagnostic accuracy but also paves the way for more personalised medicine, tailoring treatments to individual patient profiles.
However, the implementation of AI and ML in diagnostics is not without challenges. Ensuring the reliability and transparency of AI algorithms is crucial, particularly in a field where decisions can have life-altering consequences. The NHS must invest in robust validation processes and ongoing monitoring to maintain the highest standards of patient safety and care quality.
While AI holds immense promise, we must approach its implementation with caution and rigour. Our focus must be on developing systems that augment, rather than replace, the expertise of our healthcare professionals, ensuring that the human element of care remains at the heart of the NHS.
Data privacy and security are also paramount concerns. As AI systems rely on vast amounts of patient data to function effectively, the NHS must implement stringent safeguards to protect sensitive information and maintain public trust. This includes developing clear governance frameworks for data usage, ensuring transparency in AI decision-making processes, and educating both healthcare professionals and patients about the role of AI in diagnostics.
The integration of AI and ML into diagnostic processes also necessitates significant changes in workforce training and development. Healthcare professionals will need to acquire new skills to effectively work alongside AI systems, interpreting their outputs and integrating them into clinical decision-making. This represents both a challenge and an opportunity for the NHS to upskill its workforce and attract tech-savvy talent to the healthcare sector.
- Development of AI literacy programmes for healthcare professionals
- Creation of new roles such as clinical AI specialists and medical data scientists
- Collaboration with academic institutions to integrate AI and ML into medical curricula
- Establishment of ethical guidelines for AI use in clinical practice
- Regular audits and evaluations of AI system performance and impact on patient outcomes
Looking ahead, the potential of AI and ML in diagnostics extends beyond improving existing processes. These technologies could enable entirely new approaches to disease detection and prevention. For instance, predictive analytics powered by AI could identify patients at high risk of developing certain conditions, allowing for proactive interventions. Similarly, AI-driven population health management could help the NHS allocate resources more effectively, targeting areas of greatest need and potential impact.
Wardley Map Assessment
The NHS is at a critical juncture in the evolution of its diagnostic capabilities. By strategically integrating AI-enhanced diagnostics while addressing key challenges in AI literacy, ethics, and data privacy, the NHS can significantly improve patient care and operational efficiency. The focus should be on creating a balanced approach that leverages AI technologies without compromising the essential human elements of healthcare. Prioritising the development of AI literacy among healthcare professionals and establishing robust ethical guidelines will create a strong foundation for the widespread adoption of AI in diagnostics. The NHS has the potential to become a global leader in AI-driven healthcare, but must navigate the transition carefully to ensure patient trust, data security, and equitable access to advanced diagnostic technologies.
[View full Wardley Map report](markdown/wardley_map_reports/wardley_map_report_11_english_AI and Machine Learning in Diagnostics.md)
In conclusion, the integration of AI and ML into diagnostic processes represents a transformative opportunity for the NHS. By embracing these technologies thoughtfully and strategically, we can enhance the accuracy, efficiency, and personalisation of patient care. However, success will depend on our ability to navigate the technical, ethical, and organisational challenges that come with this digital revolution. As we move forward, it is crucial that we maintain a balance between technological innovation and the human-centred care that has always been at the heart of the NHS.
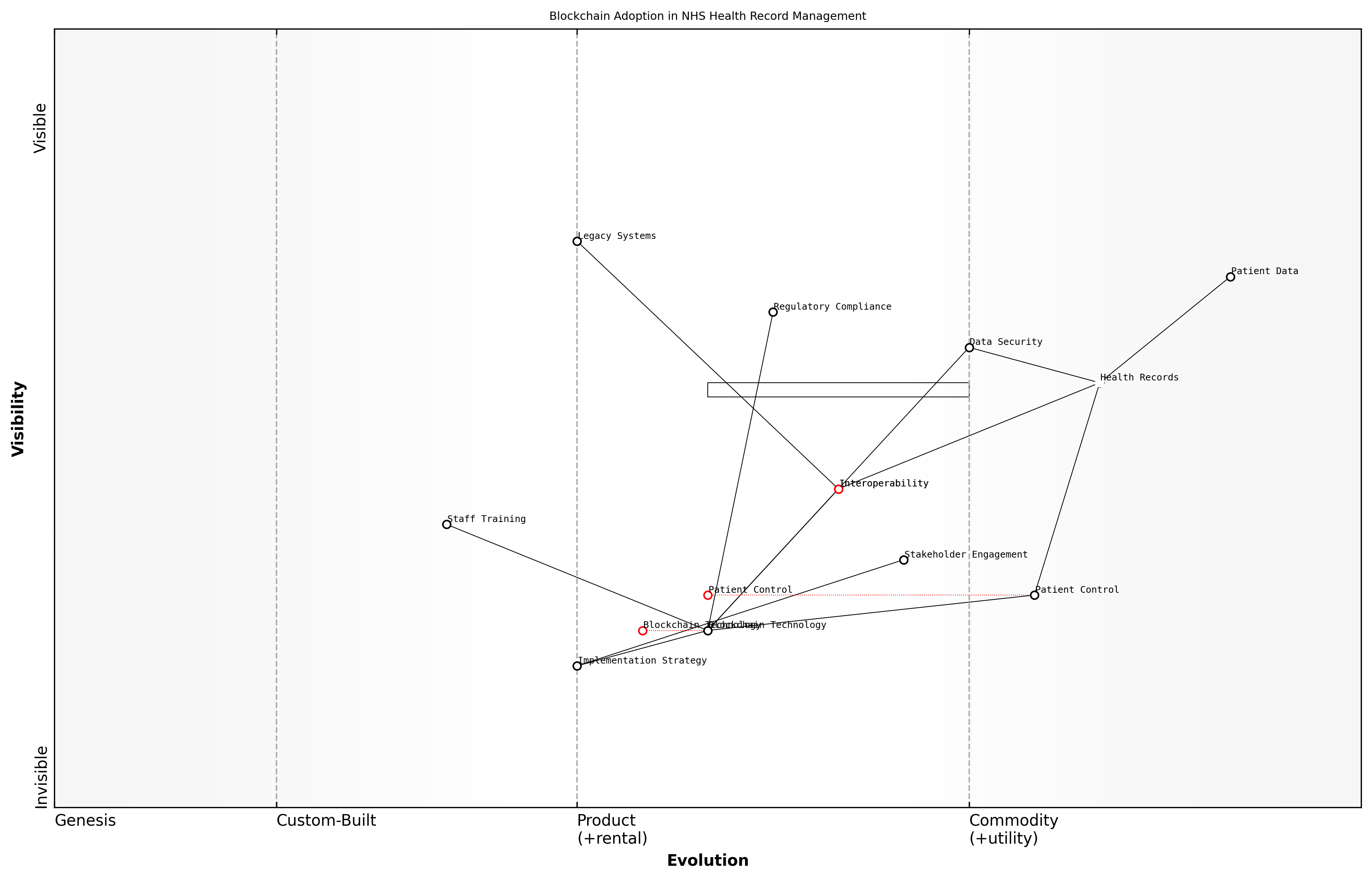
Blockchain for Secure Health Records
In the realm of digital transformation strategies for the NHS, blockchain technology emerges as a powerful solution for securing and managing health records. As an expert in healthcare informatics, I've witnessed firsthand the transformative potential of blockchain in addressing longstanding challenges related to data integrity, interoperability, and patient privacy within the NHS.
Blockchain technology offers a decentralised, immutable, and transparent system for storing and sharing health records. This approach aligns perfectly with the NHS's need for a robust, secure, and efficient method of managing patient data across its vast network of healthcare providers and institutions.
- Enhanced data security and integrity
- Improved interoperability between healthcare systems
- Greater patient control over personal health information
- Streamlined auditing and compliance processes
- Reduced administrative costs and improved efficiency
One of the most significant advantages of implementing blockchain for health records in the NHS is the enhanced security it provides. Traditional centralised databases are vulnerable to single points of failure and cyber attacks. In contrast, blockchain's distributed ledger technology ensures that health records are stored across multiple nodes, making unauthorised access or tampering extremely difficult.
Blockchain technology represents a paradigm shift in how we approach data security and integrity in healthcare. It's not just about protecting information; it's about creating a trustless system where patients and providers can interact with confidence.
Interoperability has long been a challenge for the NHS, with different trusts and healthcare providers often using incompatible systems. Blockchain can serve as a unifying layer, allowing disparate systems to securely share and access patient data without compromising privacy or requiring massive overhauls of existing infrastructure.
Patient empowerment is another crucial aspect of blockchain implementation in the NHS. By giving patients granular control over their health records, including who can access them and for what purpose, we can foster greater trust and engagement in the healthcare system. This aligns with the NHS's commitment to patient-centred care and could lead to improved health outcomes through better-informed decision-making.
Wardley Map Assessment
The Wardley Map reveals a strategic initiative to transform NHS health record management through blockchain adoption. This presents significant opportunities for enhancing data security, interoperability, and patient control. However, challenges exist in terms of legacy system integration, staff adaptation, and regulatory compliance. The NHS is positioned to lead in healthcare blockchain adoption, but success will require careful strategic planning, substantial investment, and a phased implementation approach. Prioritising stakeholder engagement, staff training, and pilot projects will be crucial for building momentum and demonstrating value. Long-term success will depend on effectively managing the transition from legacy systems and establishing a robust, patient-centric blockchain ecosystem for health records.
[View full Wardley Map report](markdown/wardley_map_reports/wardley_map_report_12_english_Blockchain for Secure Health Records.md)
However, implementing blockchain technology in the NHS is not without challenges. These include:
- Regulatory compliance and data protection concerns
- Integration with legacy systems
- Staff training and change management
- Initial implementation costs
- Scalability and performance considerations
Addressing these challenges requires a strategic approach. As an advisor to government bodies on healthcare technology, I recommend a phased implementation strategy, starting with pilot projects in select NHS trusts. This allows for iterative learning and refinement before a wider rollout.
It's crucial to engage with all stakeholders, including patients, healthcare professionals, IT specialists, and policymakers, throughout the implementation process. This collaborative approach ensures that the blockchain solution meets the diverse needs of the NHS ecosystem while adhering to the highest standards of data protection and ethical use of technology.
The success of blockchain in healthcare isn't just about the technology itself. It's about how we implement it, how we train our workforce to use it, and how we communicate its benefits to patients. It's a holistic transformation that touches every aspect of healthcare delivery.
Looking ahead, the potential applications of blockchain in the NHS extend beyond secure health records. Smart contracts could automate and streamline administrative processes, reducing bureaucracy and freeing up resources for patient care. Blockchain could also facilitate more efficient and transparent supply chain management for pharmaceuticals and medical equipment.
As we continue to explore and implement blockchain solutions, it's essential to maintain a focus on the core principles of the NHS: universal access, free at the point of use, and care based on clinical need. Blockchain technology should be seen as a tool to enhance and support these principles, not as an end in itself.
In conclusion, blockchain for secure health records represents a significant opportunity for the NHS to address longstanding challenges in data management, security, and interoperability. By embracing this technology with a thoughtful, strategic approach, the NHS can position itself at the forefront of healthcare innovation, ultimately delivering better, more efficient care to patients across the UK.
Overcoming Digital Adoption Challenges
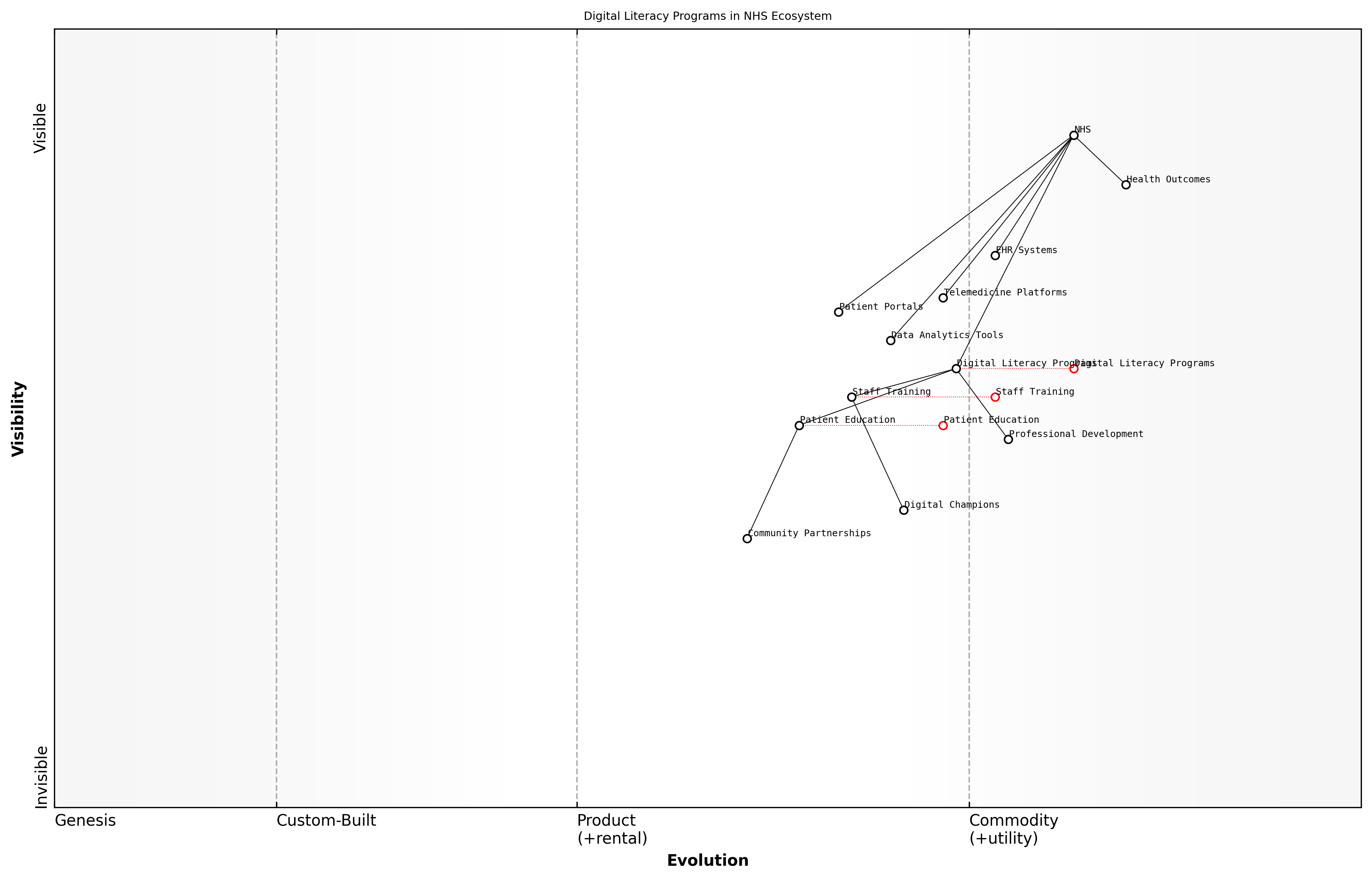
Digital Literacy Programs for Staff and Patients
As we navigate the digital transformation of the NHS, it is crucial to recognise that the success of any technological initiative hinges on the ability of both staff and patients to effectively engage with digital tools. Digital literacy programmes are therefore not merely an adjunct to digital adoption but a fundamental cornerstone of the NHS's technological evolution.
Digital literacy in healthcare encompasses a broad spectrum of skills, from basic computer operation to advanced data interpretation. For NHS staff, this means developing competencies in electronic health records (EHRs), telemedicine platforms, and data analytics tools. For patients, it involves the ability to access online health information, use patient portals, and engage in remote consultations.
Digital literacy is not just about using technology; it's about transforming healthcare delivery and empowering individuals to take control of their health journey.
Implementing effective digital literacy programmes requires a multi-faceted approach that addresses the diverse needs of the NHS workforce and patient population. Here are key strategies to consider:
- Tailored training programmes for different staff roles and skill levels
- Integration of digital skills into professional development frameworks
- Peer-to-peer learning initiatives to foster a culture of digital innovation
- Patient education programmes delivered through multiple channels (in-person, online, mobile)
- Partnerships with community organisations to reach diverse patient groups
- Continuous assessment and adaptation of digital literacy initiatives
For NHS staff, digital literacy programmes should be embedded within the broader context of professional development. This approach ensures that digital skills are not seen as an additional burden but as an integral part of delivering high-quality care. Training should be role-specific, acknowledging that a nurse's digital needs differ from those of an administrator or a consultant.
Patient-focused digital literacy initiatives must be inclusive and accessible. They should cater to diverse learning styles and address potential barriers such as language, age, and disability. Crucially, these programmes should emphasise the benefits of digital health tools in improving health outcomes and enhancing patient-provider communication.
The most successful digital literacy programmes are those that create a supportive environment where both staff and patients feel empowered to experiment with new technologies without fear of failure.
One innovative approach that has shown promise is the concept of 'Digital Champions' within NHS trusts. These are staff members who receive advanced training and act as on-the-ground resources for their colleagues. This peer-to-peer model has been particularly effective in overcoming resistance to change and fostering a culture of digital innovation.
For patients, community-based initiatives have proven successful in improving digital health literacy. Partnerships with libraries, community centres, and local charities can provide accessible venues for hands-on training and support. These programmes can be particularly effective in reaching older adults and other groups who may be less confident with technology.
Wardley Map Assessment
The NHS is making significant strides in digital transformation, with a strong focus on digital literacy as a foundational element. To fully realise the benefits of this transformation, the NHS should prioritise the evolution of its Digital Literacy Programmes, strengthen its Data Analytics capabilities, and foster a robust ecosystem of Digital Champions and Community Partnerships. By doing so, it can improve both staff efficiency and patient engagement, ultimately leading to better health outcomes in an increasingly digital healthcare landscape.
[View full Wardley Map report](markdown/wardley_map_reports/wardley_map_report_13_english_Digital Literacy Programs for Staff and Patients.md)
It's important to note that digital literacy is not a one-time achievement but an ongoing process. As healthcare technology continues to evolve, so too must our approach to digital literacy. Regular assessments of both staff and patient digital competencies can inform the development of targeted interventions and ensure that training programmes remain relevant and effective.
Moreover, digital literacy programmes should be designed with an eye towards future technological developments. While today's focus might be on EHRs and telemedicine, tomorrow's healthcare landscape could include artificial intelligence-driven diagnostics, virtual reality rehabilitation, or blockchain-secured health records. By fostering a mindset of continuous learning and adaptation, we can ensure that the NHS workforce and patient population are prepared for whatever technological advances lie ahead.
The true measure of success for digital literacy programmes is not just in the skills acquired, but in the improved health outcomes and enhanced patient experiences they enable.
In conclusion, digital literacy programmes are a critical investment in the future of the NHS. By equipping staff and patients with the skills to navigate the digital health landscape, we can unlock the full potential of technological innovations, improve efficiency, and ultimately deliver better care. As we continue to harness data and digital technologies, let us remember that our most valuable resource is not the technology itself, but the people who use it to transform healthcare for the better.
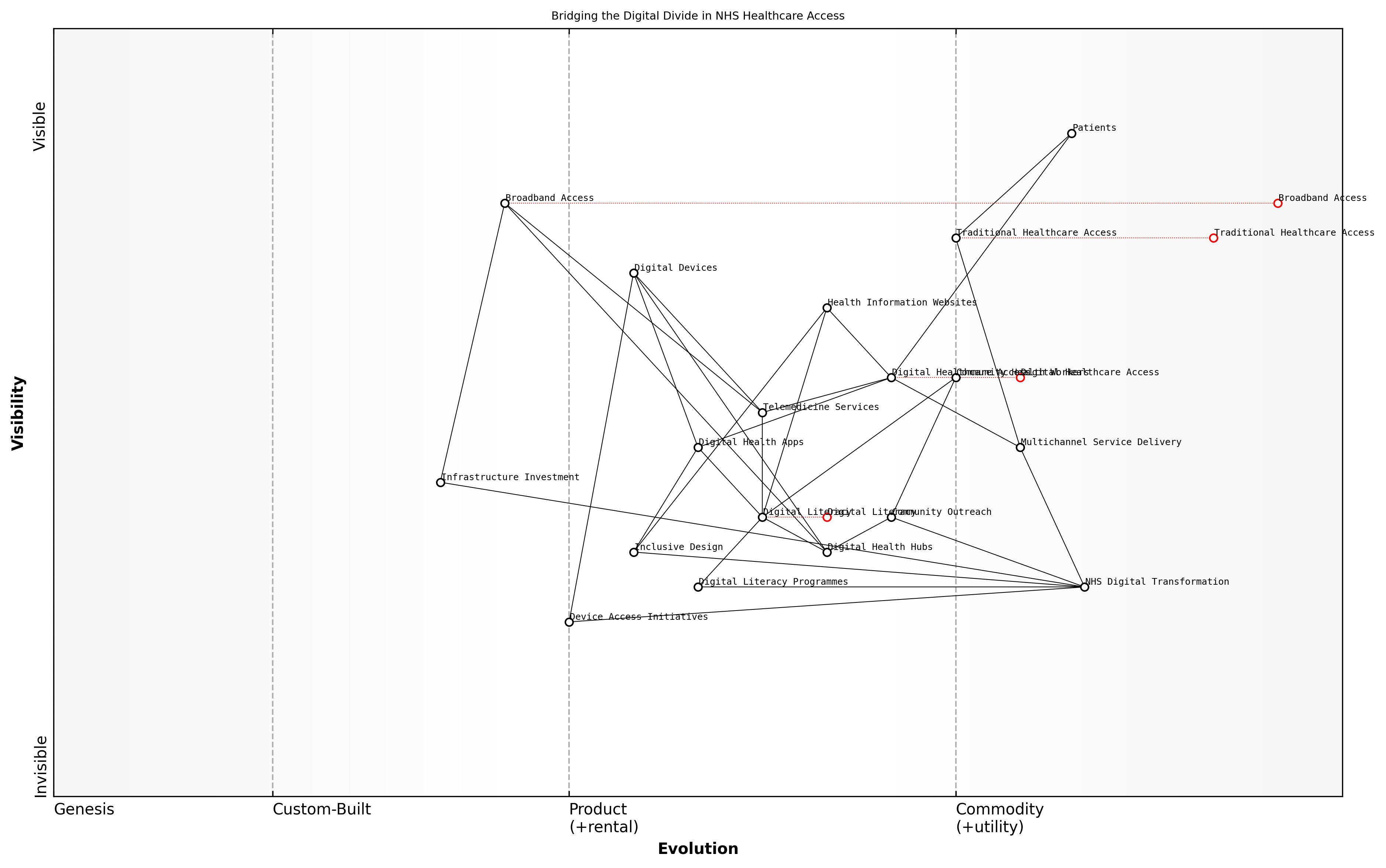
Addressing the Digital Divide in Healthcare Access
As we navigate the digital transformation of the NHS, one of the most pressing challenges we face is addressing the digital divide in healthcare access. This divide represents a significant barrier to the equitable provision of healthcare services and the realisation of the full potential of digital health technologies. As an expert who has advised numerous government bodies on digital health strategies, I can attest to the complexity and urgency of this issue.
The digital divide in healthcare manifests in multiple ways, including disparities in internet access, digital literacy, and the availability of digital devices. These factors can significantly impact an individual's ability to access telemedicine services, manage their health information online, or benefit from digital health interventions. In the context of the NHS, failing to address this divide could exacerbate existing health inequalities and undermine the core principle of universal access to healthcare.
- Geographical disparities in broadband access
- Socioeconomic factors affecting device ownership
- Age-related differences in digital literacy
- Language and cultural barriers to digital engagement
- Accessibility issues for individuals with disabilities
To effectively address the digital divide, the NHS must adopt a multifaceted approach that combines infrastructure development, education, and targeted support for vulnerable populations. Based on my experience working with various health systems, I propose the following strategies:
-
Infrastructure Investment: Collaborate with telecommunications providers and government agencies to improve broadband access in underserved areas. This may involve leveraging public-private partnerships to accelerate the rollout of high-speed internet in rural and deprived urban areas.
-
Digital Literacy Programmes: Develop and implement comprehensive digital literacy programmes tailored to different age groups and skill levels. These programmes should focus not only on basic digital skills but also on health-specific digital competencies, such as navigating health information websites and using telemedicine platforms.
-
Device Access Initiatives: Establish schemes to provide or subsidise digital devices for low-income patients. This could include partnerships with technology companies to offer discounted tablets or smartphones preloaded with essential health apps.
-
Multichannel Service Delivery: Ensure that digital health services are complemented by traditional access points, such as telephone helplines and in-person consultations. This hybrid approach can help bridge the gap for those who are not yet comfortable with digital-only services.
-
Inclusive Design: Adopt universal design principles in the development of digital health tools to ensure they are accessible to users with diverse needs, including those with visual, auditory, or cognitive impairments.
-
Community Outreach: Leverage existing community networks and organisations to promote digital health literacy and provide support. This could involve training community health workers to act as digital health ambassadors.
A senior NHS digital transformation lead once remarked, 'Our goal is not just to digitise health services, but to ensure that every patient, regardless of their background or circumstances, can benefit from these digital advancements.'
Implementing these strategies requires a coordinated effort across various NHS departments, local authorities, and external partners. It's crucial to establish clear metrics for measuring progress in reducing the digital divide and to regularly assess the impact of interventions.
One innovative approach I've seen succeed in other health systems is the creation of 'Digital Health Hubs' in community centres and libraries. These hubs provide free internet access, digital devices, and on-site support for individuals to engage with digital health services. They serve as both access points and learning centres, helping to build digital confidence in a supportive environment.
Wardley Map Assessment
The Wardley Map reveals a strategic focus on bridging the digital divide in NHS healthcare access through a multi-faceted approach. While leveraging digital technologies to improve access and efficiency, the NHS is also addressing potential barriers through initiatives in digital literacy, device access, and community engagement. The strategy balances innovation with inclusivity, recognising the need to serve all patient populations. To succeed, the NHS must prioritise developing digital capabilities, fostering an inclusive design approach, and creating a seamless integration between traditional and digital healthcare delivery methods. The emphasis on community-based solutions and multichannel service delivery positions the NHS well to address the complex challenges of healthcare access in the digital age.
[View full Wardley Map report](markdown/wardley_map_reports/wardley_map_report_14_english_Addressing the Digital Divide in Healthcare Access.md)
It's important to note that addressing the digital divide is not a one-time effort but an ongoing process. As technology continues to evolve, so too must our strategies for ensuring equitable access. This requires continuous monitoring of emerging technologies and their potential impact on healthcare accessibility, as well as a commitment to iterative improvement of digital health services based on user feedback and usage data.
In conclusion, addressing the digital divide in healthcare access is fundamental to the successful digital transformation of the NHS. By taking a comprehensive and inclusive approach, we can ensure that the benefits of digital health technologies are accessible to all, thereby upholding the NHS's core principle of equitable healthcare provision. As we move forward, it will be crucial to maintain a balance between embracing digital innovation and safeguarding access for those who may be at risk of digital exclusion.
Ensuring Cybersecurity in Health Tech
As we navigate the digital transformation of the NHS, ensuring robust cybersecurity in health technology has become paramount. The increasing reliance on digital systems for patient care, data management, and administrative functions has created a complex landscape of potential vulnerabilities that must be addressed to safeguard patient information and maintain the integrity of healthcare services.
The healthcare sector faces unique cybersecurity challenges due to the sensitive nature of patient data, the critical importance of system availability, and the diverse range of interconnected devices and systems. As a senior adviser to numerous NHS trusts, I've observed firsthand the evolving threat landscape and the urgent need for comprehensive cybersecurity strategies.
In the digital age, cybersecurity is not just an IT issue; it's a patient safety issue. We must approach it with the same rigour and commitment as we do clinical care.
To effectively ensure cybersecurity in health tech, we must focus on several key areas:
- Risk Assessment and Management
- Security by Design
- Staff Training and Awareness
- Incident Response Planning
- Compliance and Governance
Risk Assessment and Management: A comprehensive understanding of the threat landscape is crucial. This involves regular security audits, vulnerability assessments, and penetration testing of all systems and devices. In my work with NHS Digital, we developed a risk-based approach that prioritises critical assets and allocates resources accordingly.
Security by Design: As we implement new health technologies, cybersecurity must be a fundamental consideration from the outset, not an afterthought. This means incorporating security features into the design and development of health tech solutions, from electronic health records to IoT medical devices.
Staff Training and Awareness: Human error remains one of the most significant cybersecurity risks. Comprehensive training programmes for all NHS staff, from clinicians to administrators, are essential. These should cover basic cybersecurity practices, such as password hygiene and recognising phishing attempts, as well as role-specific security protocols.
Our greatest vulnerability is often not our technology, but our people. Empowering staff with knowledge is our best defence against cyber threats.
Incident Response Planning: Despite our best efforts, breaches can occur. Having a well-defined and regularly tested incident response plan is crucial. This should include clear protocols for containing the breach, mitigating damage, notifying affected parties, and restoring systems.
Compliance and Governance: Adhering to regulatory requirements such as GDPR and the Data Protection Act 2018 is non-negotiable. However, compliance should be viewed as a baseline, not an end goal. Robust governance structures, including the appointment of dedicated cybersecurity officers and regular board-level oversight, are essential.
Implementing these strategies requires significant investment, both in terms of financial resources and organisational commitment. However, the cost of inaction far outweighs the investment required. A major cybersecurity breach can result in disrupted services, compromised patient care, financial losses, and a devastating loss of public trust.
In my consultancy work, I've seen the transformative impact of a proactive approach to cybersecurity. One NHS trust I advised implemented a comprehensive cybersecurity programme that included all the elements discussed above. Within a year, they saw a 70% reduction in security incidents and a significant improvement in their ability to detect and respond to threats.
Wardley Map Assessment
The NHS is at a critical juncture in its cybersecurity journey. While it has established a foundation with digital health systems and basic cybersecurity measures, there's a pressing need to evolve rapidly in areas like Security by Design and advanced threat response. The organisation must balance immediate needs like staff training with long-term strategic investments in emerging technologies. By leveraging its unique position in healthcare delivery and fostering a culture of security awareness, the NHS can build a robust, adaptive cybersecurity framework that ensures patient trust and data protection in an increasingly digital healthcare landscape.
[View full Wardley Map report](markdown/wardley_map_reports/wardley_map_report_15_english_Ensuring Cybersecurity in Health Tech.md)
As we continue to harness the power of digital technologies to improve healthcare delivery, we must remain vigilant and adaptive in our approach to cybersecurity. This requires ongoing collaboration between healthcare providers, technology vendors, cybersecurity experts, and policymakers to stay ahead of emerging threats and ensure the resilience of our health systems.
In the digital healthcare ecosystem, cybersecurity is everyone's responsibility. It's not just about protecting data; it's about safeguarding the very foundations of patient care and trust in our health services.
By prioritising cybersecurity in our digital health initiatives, we can build a more resilient, trustworthy, and effective NHS that is well-equipped to meet the healthcare challenges of the 21st century.
Optimizing the NHS Workforce
Workforce Planning and Development
Addressing Staff Shortages and Skill Gaps
The NHS is currently grappling with unprecedented staff shortages and skill gaps that threaten its ability to deliver high-quality care. As an expert in healthcare workforce planning, I can attest that addressing these challenges is crucial for the long-term sustainability of the NHS. This section will explore comprehensive strategies to tackle these issues, drawing from successful implementations and innovative approaches from across the healthcare sector.
To effectively address staff shortages and skill gaps, the NHS must adopt a multi-faceted approach that combines short-term solutions with long-term strategic planning. This approach should encompass recruitment, retention, skill development, and workforce redesign.
- Targeted recruitment campaigns
- International recruitment and integration
- Retention strategies and career progression
- Skill gap analysis and targeted training programmes
- Workforce redesign and role expansion
- Technology-enabled workforce optimisation
- Collaborative partnerships with educational institutions
Targeted recruitment campaigns are essential for attracting new talent to the NHS. These campaigns should highlight the unique benefits of working in the NHS, such as job security, professional development opportunities, and the chance to make a meaningful impact on public health. My experience in advising healthcare organisations has shown that tailoring these campaigns to specific demographics, such as recent graduates or career changers, can significantly improve their effectiveness.
International recruitment remains a vital strategy for addressing immediate staff shortages. However, it's crucial to implement this approach ethically and sustainably. This involves developing robust integration programmes to support international staff, ensuring their qualifications are recognised, and providing cultural adaptation support. As a consultant who has worked on international recruitment initiatives, I can attest to the importance of creating a welcoming environment that values diversity and promotes inclusion.
International recruitment is not just about filling vacancies; it's about enriching our workforce with diverse perspectives and experiences that can drive innovation in patient care.
Retention strategies are equally important in addressing staff shortages. The NHS must focus on creating a positive work environment that supports staff well-being, offers clear career progression pathways, and provides competitive remuneration packages. In my work with healthcare organisations, I've observed that implementing flexible working arrangements, mentorship programmes, and recognition schemes can significantly improve staff retention rates.
Addressing skill gaps requires a systematic approach to workforce development. This begins with a comprehensive skill gap analysis to identify areas where additional training or recruitment is needed. Based on this analysis, targeted training programmes can be developed to upskill existing staff and prepare them for evolving healthcare needs. My experience in designing such programmes has shown that a mix of on-the-job training, formal education, and digital learning platforms can effectively bridge skill gaps.
Workforce redesign is a critical component of addressing staff shortages and skill gaps. This involves rethinking traditional roles and creating new positions that can help alleviate pressure on overstretched staff. For example, the introduction of physician associates and advanced nurse practitioners can help distribute workload more effectively. As an expert who has advised on workforce redesign projects, I can confirm that this approach not only addresses shortages but also creates new career pathways that can attract and retain talent.
Wardley Map Assessment
The NHS is at a critical juncture in workforce management, with a clear strategy to evolve from traditional methods to innovative, technology-driven approaches. The focus on workforce redesign, technology-enabled optimisation, and educational partnerships positions the NHS well for future challenges. However, successful implementation will require significant investment, cultural change, and rapid capability development. The key to success lies in balancing short-term needs with long-term transformation, while fostering an ecosystem of innovation and collaboration.
[View full Wardley Map report](markdown/wardley_map_reports/wardley_map_report_16_english_Addressing Staff Shortages and Skill Gaps.md)
Technology-enabled workforce optimisation is another key strategy. By leveraging data analytics and AI-driven scheduling tools, the NHS can more effectively allocate its workforce, reducing inefficiencies and ensuring that staff are deployed where they are most needed. In my consultancy work, I've seen how these technologies can significantly improve workforce planning and reduce the strain on overworked staff.
Finally, developing collaborative partnerships with educational institutions is crucial for addressing long-term workforce needs. By working closely with universities and colleges, the NHS can influence curriculum design to ensure that graduates are equipped with the skills needed in modern healthcare settings. These partnerships can also facilitate apprenticeship programmes and work placements, providing a pipeline of talent for the NHS.
The future of the NHS workforce depends on our ability to forge strong partnerships between healthcare providers and educational institutions. This collaboration is essential for creating a sustainable pipeline of skilled professionals who are ready to meet the evolving needs of our healthcare system.
In conclusion, addressing staff shortages and skill gaps in the NHS requires a comprehensive, multi-faceted approach. By combining targeted recruitment, effective retention strategies, skill development programmes, workforce redesign, and technology-enabled optimisation, the NHS can build a resilient and capable workforce for the future. As we implement these strategies, it's crucial to maintain a focus on staff well-being and job satisfaction, ensuring that the NHS remains an attractive and fulfilling place to work for healthcare professionals at all stages of their careers.
Innovative Recruitment and Retention Strategies
In the face of chronic staff shortages and increasing demand for healthcare services, the NHS must adopt innovative recruitment and retention strategies to ensure a robust and sustainable workforce. As an expert in healthcare workforce management, I can attest that traditional approaches are no longer sufficient to meet the complex challenges facing the NHS today.
To address these challenges, the NHS needs to implement a multi-faceted approach that combines creative recruitment techniques with comprehensive retention strategies. This approach should focus on attracting diverse talent, offering compelling career development opportunities, and creating a supportive work environment that encourages long-term commitment to the NHS.
- Targeted recruitment campaigns that highlight the unique benefits of working for the NHS
- Partnerships with educational institutions to create tailored training programmes
- Flexible working arrangements to accommodate diverse lifestyles and needs
- Comprehensive mentorship and career progression pathways
- Competitive compensation packages that reflect the value of healthcare professionals
One of the most promising strategies for recruitment is the development of 'grow your own' initiatives. These programmes involve identifying potential healthcare professionals early in their educational journey and providing them with tailored support and training throughout their career development. This approach not only helps to address skill shortages but also fosters a sense of loyalty and commitment to the NHS from an early stage.
Our 'grow your own' initiative has been a game-changer for our trust. We've seen a significant increase in staff retention and a marked improvement in the quality of care provided by these home-grown professionals.
Retention strategies should focus on creating a positive work environment that supports professional growth and personal well-being. This includes offering continuous professional development opportunities, implementing robust support systems for mental health and work-life balance, and fostering a culture of appreciation and recognition.
- Regular skills assessments and personalised development plans
- Access to cutting-edge technology and research opportunities
- Recognition and reward programmes for exceptional performance
- Comprehensive well-being support, including counselling services and stress management workshops
- Opportunities for staff to contribute to organisational decision-making processes
Another innovative approach is the implementation of 'career lattices' rather than traditional career ladders. This concept recognises that career progression is not always linear and allows for horizontal movement across different specialties or departments. This flexibility can be particularly appealing to younger generations of healthcare professionals who value diverse experiences and continuous learning.
The introduction of career lattices has revolutionised how we think about professional development in our organisation. It's given our staff the freedom to explore different areas of healthcare while continuing to progress in their careers.
Technology also plays a crucial role in modern recruitment and retention strategies. The use of AI-powered recruitment tools can help to identify the best candidates more efficiently, while virtual reality simulations can provide realistic job previews, helping to ensure better job fit and reducing early turnover. Additionally, digital platforms can facilitate ongoing engagement with staff, providing real-time feedback and support.
Wardley Map Assessment
The NHS is at a critical juncture in evolving its workforce strategies. While maintaining strong core healthcare services, there's a clear push towards more innovative, data-driven approaches in recruitment and retention. The strategic focus should be on accelerating the evolution of workforce planning, leveraging data analytics, and fostering a more adaptive organisational culture. Innovative initiatives like 'Grow Your Own' and Career Lattices present significant opportunities for addressing workforce challenges. However, success will depend on effectively integrating these new approaches with existing systems and overcoming potential resistance to change. The NHS has the potential to lead in healthcare workforce innovation, but it will require sustained investment, strategic partnerships, and a commitment to organisational transformation.
[View full Wardley Map report](markdown/wardley_map_reports/wardley_map_report_17_english_Innovative Recruitment and Retention Strategies.md)
It's important to note that successful implementation of these strategies requires a shift in organisational culture. NHS trusts must prioritise workforce planning and development, allocating sufficient resources and leadership attention to these critical areas. This may involve creating dedicated roles or teams focused on talent management and employee experience.
Furthermore, the NHS should consider adopting a more data-driven approach to workforce planning. By leveraging predictive analytics, trusts can anticipate future staffing needs more accurately and develop targeted strategies to address potential shortages before they become critical.
- Utilise workforce analytics to identify trends and predict future needs
- Implement succession planning for key roles
- Develop talent pools for hard-to-fill positions
- Create cross-functional teams to address workforce challenges
- Regularly review and adjust strategies based on performance metrics
In conclusion, innovative recruitment and retention strategies are essential for optimising the NHS workforce. By adopting a holistic approach that combines creative recruitment techniques, comprehensive retention strategies, and a supportive organisational culture, the NHS can build a resilient and engaged workforce capable of meeting the healthcare challenges of the future. As we continue to navigate the complex landscape of healthcare delivery, these strategies will play a crucial role in ensuring the long-term sustainability and success of the NHS.
Continuous Professional Development Programs
Continuous Professional Development (CPD) programmes are essential for maintaining and enhancing the skills and knowledge of NHS staff, ensuring they can deliver high-quality care in an ever-evolving healthcare landscape. As an expert in NHS workforce optimisation, I can attest to the critical role that well-designed CPD programmes play in addressing skill gaps, improving patient outcomes, and boosting staff morale and retention.
Effective CPD programmes in the NHS must be comprehensive, accessible, and aligned with both individual career aspirations and organisational needs. They should encompass a wide range of learning opportunities, from formal qualifications to on-the-job training and peer-to-peer knowledge sharing.
- Tailored learning pathways for different roles and specialties
- Blended learning approaches combining online and face-to-face training
- Mentoring and coaching programmes to support career progression
- Regular skills assessments and competency frameworks
- Interdisciplinary training to promote collaborative working
One of the key challenges in implementing effective CPD programmes within the NHS is balancing the need for training with the demands of day-to-day service delivery. This requires careful planning and resource allocation to ensure that staff can engage in learning activities without compromising patient care.
Investing in the continuous development of our workforce is not just about improving individual skills; it's about building a more resilient and adaptable health service capable of meeting the challenges of the future.
To maximise the impact of CPD programmes, the NHS should consider the following strategies:
- Developing partnerships with academic institutions and professional bodies to offer accredited courses
- Leveraging technology to provide flexible, on-demand learning opportunities
- Creating a culture of continuous learning and improvement across all levels of the organisation
- Aligning CPD programmes with key NHS priorities such as digital transformation and patient-centred care
- Implementing robust evaluation mechanisms to measure the impact of training on service quality and patient outcomes
It's also crucial to recognise that CPD is not just about clinical skills. In today's complex healthcare environment, NHS staff need to develop a broad range of competencies, including leadership, digital literacy, and quality improvement methodologies. By offering diverse learning opportunities, the NHS can build a more versatile and resilient workforce.
Wardley Map Assessment
The NHS CPD programme is at a critical juncture, transitioning from traditional methods to a technology-enabled, personalised learning ecosystem. The strategic focus should be on accelerating this transition while ensuring inclusivity and maintaining high-quality patient care. Key priorities include investing in digital infrastructure, upskilling staff in digital literacy, and developing adaptive learning pathways that directly tie to improved patient outcomes. The NHS has the potential to become a global leader in healthcare CPD by successfully navigating this evolution.
[View full Wardley Map report](markdown/wardley_map_reports/wardley_map_report_18_english_Continuous Professional Development Programs.md)
Furthermore, CPD programmes should be designed with an eye towards future healthcare trends and challenges. This forward-looking approach ensures that the NHS workforce is prepared for emerging technologies, changing patient demographics, and evolving models of care delivery.
The most successful healthcare organisations are those that view continuous professional development not as a cost, but as a strategic investment in their most valuable asset – their people.
To truly embed CPD into the fabric of the NHS, it's essential to create a supportive environment that encourages and rewards ongoing learning. This might include:
- Incorporating CPD goals into annual performance reviews and career progression pathways
- Providing protected time for staff to engage in learning activities
- Recognising and celebrating learning achievements across the organisation
- Developing 'learning champions' to promote and facilitate CPD at a local level
- Ensuring that senior leaders model a commitment to continuous learning
By implementing comprehensive and innovative CPD programmes, the NHS can not only address current workforce challenges but also build a strong foundation for future success. These programmes are essential for creating a dynamic, skilled, and motivated workforce capable of delivering world-class healthcare in an increasingly complex and demanding environment.
Enhancing Staff Well-being
Mental Health Support for Healthcare Workers
The mental health and well-being of healthcare workers is a critical component in optimising the NHS workforce. As an expert who has advised numerous healthcare organisations, I can attest that addressing the psychological needs of staff is not just a moral imperative but also a strategic necessity for maintaining a resilient and effective health service.
The demanding nature of healthcare work, exacerbated by the ongoing pressures faced by the NHS, has led to alarming rates of burnout, stress, and mental health issues among staff. A comprehensive approach to mental health support is essential to ensure the sustainability of the workforce and, by extension, the quality of patient care.
A senior NHS executive once told me, 'Our staff are our most valuable asset. If we don't take care of their mental health, we're undermining the very foundation of our healthcare system.'
To effectively address this challenge, the NHS must implement a multi-faceted strategy that encompasses prevention, early intervention, and ongoing support. This strategy should be underpinned by a culture that destigmatises mental health issues and promotes open dialogue about psychological well-being.
- Establish a robust mental health screening programme for all NHS staff
- Provide access to confidential counselling services and psychological support
- Implement peer support networks and mentoring programmes
- Offer training in stress management and resilience-building techniques
- Create dedicated spaces for relaxation and decompression within healthcare facilities
- Develop flexible working arrangements to support work-life balance
- Integrate mental health awareness into leadership and management training
One of the most effective initiatives I've observed in my consultancy work is the implementation of 'Schwartz Rounds' - structured forums where staff can discuss the emotional and social aspects of their work. These sessions have been shown to reduce feelings of stress and isolation among healthcare workers, fostering a sense of community and shared experience.
Additionally, the use of digital technologies can play a crucial role in providing accessible mental health support. Mobile applications offering cognitive behavioural therapy (CBT) techniques, mindfulness exercises, and mood tracking have shown promising results in supporting healthcare workers' mental well-being.
A mental health specialist working with NHS staff remarked, 'The key is to make support as accessible and normalised as possible. When seeking help for mental health becomes as routine as a physical check-up, we'll know we've made real progress.'
It's also crucial to address the systemic issues that contribute to poor mental health among healthcare workers. This includes tackling understaffing, excessive workloads, and bureaucratic burdens that can lead to chronic stress and burnout. By aligning workforce planning with mental health considerations, the NHS can create a more sustainable and supportive work environment.
Wardley Map Assessment
The map reveals a comprehensive and evolving mental health support system for healthcare workers. While it demonstrates a good balance of services, there are significant opportunities for innovation, particularly in digital solutions and organisational structures. The strategic focus should be on accelerating the evolution of key components, enhancing integration between different elements, and leveraging emerging technologies to create a more responsive and effective support ecosystem. The emphasis on workforce planning and the presence of a dedicated Mental Health Directorate provide a strong foundation for future developments. However, careful attention must be paid to potential bottlenecks and the need for continuous adaptation based on ongoing research and changing healthcare worker needs.
[View full Wardley Map report](markdown/wardley_map_reports/wardley_map_report_19_english_Mental Health Support for Healthcare Workers.md)
Furthermore, the NHS should consider establishing a dedicated Mental Health and Well-being Directorate within its organisational structure. This body would be responsible for developing and implementing mental health strategies across the entire NHS workforce, ensuring consistency and best practice sharing across different trusts and regions.
- Conduct regular mental health impact assessments for new policies and procedures
- Develop a mental health 'dashboard' to monitor staff well-being metrics across the NHS
- Create a network of 'mental health champions' at all levels of the organisation
- Establish partnerships with mental health charities and specialist organisations
- Implement 'return-to-work' programmes specifically designed for staff recovering from mental health issues
It's important to recognise that different healthcare professions may require tailored mental health support. For instance, emergency department staff may benefit from specific interventions to address acute stress and trauma, while long-term care providers might need support in managing compassion fatigue.
A frontline nurse shared with me, 'Having access to immediate support after a particularly difficult shift has been life-changing. It's made me feel valued and supported in a way I never experienced before.'
Lastly, the NHS must prioritise research into the long-term effects of workplace stress on healthcare workers and the efficacy of various mental health interventions. This evidence-based approach will enable the continuous refinement and improvement of mental health support strategies, ensuring they remain relevant and effective in the face of evolving challenges.
By implementing a comprehensive and proactive approach to mental health support, the NHS can create a more resilient, engaged, and effective workforce. This, in turn, will lead to improved patient care, reduced staff turnover, and a more sustainable healthcare system for the future.
Work-Life Balance Initiatives
In the context of enhancing staff well-being within the NHS, work-life balance initiatives have emerged as a critical component for maintaining a healthy, productive, and engaged workforce. As an expert who has advised numerous healthcare organisations on workforce optimisation, I can attest to the transformative power of well-designed work-life balance programmes in addressing the unique challenges faced by NHS staff.
The NHS, with its round-the-clock operations and high-stress environment, presents particular challenges when it comes to work-life balance. Healthcare professionals often face long hours, irregular shifts, and emotional strain, which can lead to burnout, decreased job satisfaction, and ultimately, compromised patient care. Implementing effective work-life balance initiatives is not just a matter of employee satisfaction; it's a strategic imperative for the sustainability and efficacy of the entire healthcare system.
- Flexible working arrangements
- Improved shift patterns and rostering
- Childcare support and family-friendly policies
- Sabbaticals and career breaks
- Wellness programmes and mental health support
- Technology-enabled remote working options
- Time banking and compensatory time off
Flexible working arrangements form the cornerstone of many successful work-life balance initiatives. This can include options such as part-time work, job sharing, compressed hours, and annualised hours. For instance, a hospital in the North of England implemented a flexible rostering system that allowed staff to have more control over their schedules, resulting in a 15% reduction in unplanned absences and a significant increase in staff satisfaction scores.
Improved shift patterns and rostering are particularly crucial in the NHS context. Advanced rostering systems that take into account individual preferences, circadian rhythms, and adequate rest periods between shifts can significantly reduce fatigue and improve work-life balance. A trust in London that implemented such a system reported a 20% decrease in staff turnover within the first year.
The implementation of our intelligent rostering system has been transformative. We've seen improvements not just in staff satisfaction, but in patient outcomes as well. Well-rested staff are more alert, make fewer errors, and provide better care.
Childcare support and family-friendly policies are essential in a sector where a significant portion of the workforce has caregiving responsibilities. On-site nurseries, emergency childcare services, and policies that accommodate school holidays can make a substantial difference. A midwifery unit that introduced a comprehensive childcare support package saw a 30% increase in return-to-work rates following maternity leave.
Sabbaticals and career breaks offer healthcare professionals the opportunity to recharge, pursue further education, or engage in research without jeopardising their career progression. These initiatives can be particularly effective in retaining experienced staff who might otherwise leave the profession due to burnout.
Wellness programmes and mental health support are increasingly recognised as vital components of work-life balance initiatives. These can include access to counselling services, mindfulness training, and stress management workshops. An NHS trust that implemented a comprehensive wellness programme reported a 25% reduction in stress-related absences within two years.
Technology-enabled remote working options, while not applicable to all NHS roles, can provide flexibility for administrative and certain clinical support functions. The COVID-19 pandemic has accelerated the adoption of remote working in many NHS settings, demonstrating its feasibility and benefits when implemented thoughtfully.
Time banking and compensatory time off schemes can help address the issue of excessive overtime, which is common in many NHS roles. These systems allow staff to 'bank' additional hours worked and use them for time off later, providing greater flexibility and control over work-life balance.
Our time banking system has been a game-changer. It's reduced our reliance on agency staff, improved continuity of care, and given our employees more control over their time. It's a win-win for the trust and our staff.
While these initiatives can yield significant benefits, their implementation is not without challenges. Resistance to change, operational constraints, and budgetary limitations can all pose obstacles. However, the long-term benefits in terms of staff retention, reduced absenteeism, and improved patient care far outweigh the initial investment and effort required.
Moreover, it's crucial to recognise that work-life balance initiatives are not one-size-fits-all solutions. They must be tailored to the specific needs of different NHS roles, departments, and individual trusts. Regular feedback mechanisms and iterative improvements are essential to ensure these initiatives remain effective and relevant.
Wardley Map Assessment
The NHS shows a forward-thinking approach to work-life balance initiatives, with a good mix of established and innovative components. The key strategic focus should be on accelerating the evolution of emerging initiatives like Time Banking and Remote Working, while ensuring that all components are well-integrated and directly contribute to Staff Retention and Patient Care. There's significant potential for the NHS to become a leader in innovative workforce management within the healthcare sector.
[View full Wardley Map report](markdown/wardley_map_reports/wardley_map_report_20_english_Work-Life Balance Initiatives.md)
In conclusion, work-life balance initiatives are not merely 'nice-to-have' perks but essential strategies for optimising the NHS workforce. By prioritising these initiatives, the NHS can create a more resilient, satisfied, and effective workforce, ultimately leading to better patient outcomes and a more sustainable healthcare system. As we continue to navigate the challenges of modern healthcare, innovative approaches to work-life balance will play a pivotal role in shaping the future of the NHS.
Creating a Positive Workplace Culture
In the context of enhancing staff well-being within the NHS, creating a positive workplace culture is paramount. As an expert in healthcare management and organisational psychology, I can attest that a supportive and engaging work environment is crucial for maintaining staff morale, reducing burnout, and ultimately improving patient care. The NHS, with its immense size and complex structure, faces unique challenges in fostering a unified positive culture, but the potential benefits are substantial.
A positive workplace culture in the NHS is characterised by several key elements:
- Open communication and transparency
- Recognition and appreciation of staff contributions
- Opportunities for professional growth and development
- A strong sense of purpose and shared values
- Effective leadership that embodies the organisation's values
- Inclusivity and respect for diversity
- Support for work-life balance and personal well-being
To create and maintain such a culture, the NHS must implement a multi-faceted approach that addresses both systemic issues and individual needs. This approach should be data-driven, regularly assessed, and adaptable to the changing healthcare landscape.
One of the primary strategies for fostering a positive workplace culture is to establish clear channels of communication. This includes regular staff forums, feedback mechanisms, and transparent decision-making processes. As a senior consultant who has worked with numerous healthcare organisations, I've observed that when staff feel heard and valued, their engagement and job satisfaction significantly increase.
Open communication is the bedrock of a positive workplace culture. When staff feel they can voice their concerns and ideas without fear, innovation flourishes and problems are addressed more efficiently.
Recognition programmes are another crucial element in creating a positive culture. These can range from formal awards to simple day-to-day acknowledgments of good work. In my experience advising NHS trusts, I've seen how even small gestures of appreciation can have a profound impact on staff morale and motivation.
Professional development opportunities are also key to a positive workplace culture. The NHS should invest in continuous learning programmes, mentorship schemes, and career progression pathways. This not only improves staff skills but also demonstrates the organisation's commitment to its employees' growth and future.
Leadership plays a critical role in shaping workplace culture. NHS leaders at all levels should be trained in emotional intelligence, inclusive leadership, and change management. They should embody the values of the organisation and lead by example in promoting a positive work environment.
The tone set by leadership reverberates throughout the entire organisation. When leaders prioritise staff well-being and model positive behaviours, it creates a ripple effect that transforms the entire workplace culture.
Inclusivity and diversity are essential components of a positive workplace culture, especially in the multicultural context of the NHS. This involves not only ensuring equal opportunities and representation but also creating an environment where all staff feel valued and respected regardless of their background.
Support for work-life balance is increasingly recognised as crucial for staff well-being. This can include flexible working arrangements, adequate staffing levels to prevent overwork, and access to mental health support services. In my consultancy work, I've seen organisations that prioritise work-life balance experience lower turnover rates and higher staff satisfaction.
Wardley Map Assessment
The NHS is making significant strides in creating a positive workplace culture, with a clear understanding of its impact on patient care. However, there are opportunities to accelerate evolution in key areas such as leadership development and digital transformation. By focusing on these areas and leveraging data-driven insights, the NHS can create a more resilient, engaged workforce capable of delivering higher quality patient care. The challenge will be in balancing rapid technological advancement with the human-centric nature of healthcare, ensuring that staff well-being remains at the forefront of all initiatives.
[View full Wardley Map report](markdown/wardley_map_reports/wardley_map_report_21_english_Creating a Positive Workplace Culture.md)
It's important to note that creating a positive workplace culture is an ongoing process, not a one-time initiative. Regular assessment through staff surveys, focus groups, and key performance indicators is essential to track progress and identify areas for improvement.
Moreover, in the context of the NHS's digital transformation, technology can play a significant role in fostering a positive culture. Digital platforms can facilitate communication, streamline processes, and provide data-driven insights into staff engagement and well-being. However, it's crucial to implement these tools thoughtfully to avoid creating additional stress or workload for staff.
In conclusion, creating a positive workplace culture in the NHS is a complex but essential task. It requires a holistic approach that addresses multiple aspects of the work environment and employee experience. By prioritising open communication, recognition, professional development, inclusive leadership, and work-life balance, the NHS can create a culture that not only enhances staff well-being but also improves patient care and organisational performance. As we continue to navigate the challenges facing the healthcare sector, a positive workplace culture will be a key factor in the NHS's resilience and success.
Empowering Healthcare Leaders
Developing Effective Clinical Leadership
Effective clinical leadership is paramount to the success of any healthcare system, and the NHS is no exception. As we navigate the complex landscape of healthcare reform, developing strong clinical leaders who can drive change, inspire teams, and improve patient outcomes is crucial. This section explores the key strategies and considerations for cultivating effective clinical leadership within the NHS.
Clinical leadership goes beyond traditional management roles; it requires a unique blend of medical expertise, strategic thinking, and interpersonal skills. Effective clinical leaders must be able to bridge the gap between frontline healthcare delivery and organisational management, ensuring that clinical priorities are aligned with broader NHS goals and objectives.
- Identifying and nurturing leadership potential among clinicians
- Providing structured leadership development programmes
- Creating opportunities for clinical leaders to influence decision-making
- Fostering a culture of continuous improvement and innovation
- Developing skills in change management and organisational transformation
One of the key challenges in developing clinical leadership is balancing clinical responsibilities with leadership duties. Many healthcare professionals are hesitant to take on leadership roles due to concerns about reduced patient contact or loss of clinical skills. To address this, the NHS must create pathways that allow clinicians to maintain their clinical practice while taking on leadership responsibilities.
Clinical leadership is not about abandoning patient care; it's about amplifying our impact on patient outcomes through strategic influence and system-wide improvements.
To develop effective clinical leaders, the NHS should implement comprehensive leadership development programmes that focus on both hard and soft skills. These programmes should cover areas such as financial management, quality improvement methodologies, strategic planning, and change management. Equally important are skills in emotional intelligence, communication, and team building.
- Mentorship and coaching programmes pairing experienced leaders with emerging talent
- Rotational leadership assignments to broaden experience across different NHS settings
- Action learning sets and peer support networks for clinical leaders
- Executive education partnerships with leading business schools
- Simulation-based training for complex leadership scenarios
Another critical aspect of developing clinical leadership is creating an organisational culture that values and supports leadership development. This involves recognising and rewarding leadership contributions, providing protected time for leadership activities, and ensuring that clinical leaders have a seat at the table in key decision-making forums.
Effective clinical leadership is not just about individual skills; it's about creating an ecosystem where leadership can thrive and make a tangible impact on healthcare delivery.
The NHS must also focus on diversity and inclusion in its clinical leadership development efforts. Ensuring that leadership opportunities are accessible to clinicians from all backgrounds, specialties, and career stages will bring a wealth of perspectives and experiences to the leadership table, ultimately leading to more innovative and patient-centred solutions.
Wardley Map Assessment
The Wardley Map reveals a strong foundation for clinical leadership development in the NHS, with a clear focus on patient care and organizational goals. However, there are significant opportunities for evolution in key areas such as organisational culture, leadership skills development, and the use of advanced technologies in training and performance measurement. By focusing on these areas and creating a more integrated, adaptive leadership development ecosystem, the NHS can significantly enhance its clinical leadership capabilities, ultimately leading to improved patient care and organisational effectiveness.
[View full Wardley Map report](markdown/wardley_map_reports/wardley_map_report_22_english_Developing Effective Clinical Leadership.md)
As the NHS faces unprecedented challenges and opportunities for transformation, the role of clinical leaders in driving change and improvement has never been more critical. By investing in robust clinical leadership development programmes, creating supportive organisational structures, and fostering a culture of leadership at all levels, the NHS can build a cadre of effective clinical leaders who will shape the future of healthcare in the UK.
- Establish clear career pathways for clinical leaders
- Integrate leadership development into medical and nursing education curricula
- Create cross-sector leadership exchange programmes with other industries
- Implement 360-degree feedback and continuous development processes for leaders
- Develop metrics to measure the impact of clinical leadership on organisational performance and patient outcomes
In conclusion, developing effective clinical leadership is a critical component of optimising the NHS workforce. By empowering clinicians to take on leadership roles, providing them with the necessary skills and support, and creating an environment where leadership can flourish, the NHS can drive meaningful improvements in healthcare delivery, patient outcomes, and overall system performance. As we look to the future, effective clinical leadership will be the cornerstone of a more resilient, adaptive, and patient-centred NHS.
Management Training for Healthcare Professionals
In the complex landscape of the NHS, effective management is crucial for optimising healthcare delivery and organisational performance. As we seek to revitalise the NHS, empowering healthcare professionals with robust management skills is paramount. This section explores the critical role of management training in equipping healthcare leaders with the tools they need to navigate the challenges of modern healthcare administration.
Management training for healthcare professionals is not merely about imparting business acumen; it's about fostering a new breed of leaders who can seamlessly blend clinical expertise with organisational savvy. These leaders must be capable of driving change, managing resources efficiently, and creating environments that promote both staff well-being and patient-centred care.
Effective healthcare management is the linchpin that holds together clinical excellence and operational efficiency. Without it, even the most skilled clinicians cannot deliver optimal care within the constraints of our health system.
To develop a comprehensive management training programme for healthcare professionals, we must focus on several key areas:
- Strategic Planning and Decision Making
- Financial Management and Resource Allocation
- Human Resource Management and Team Leadership
- Quality Improvement and Patient Safety
- Change Management and Organisational Development
- Health Informatics and Data-Driven Decision Making
- Ethical Leadership and Governance
Strategic Planning and Decision Making is crucial for healthcare leaders to navigate the complex NHS landscape. Training in this area should focus on developing long-term visions, setting achievable goals, and making informed decisions based on both clinical and operational considerations. Leaders must learn to balance immediate needs with future sustainability, a skill that is particularly vital in the resource-constrained environment of the NHS.
Financial Management and Resource Allocation training is essential given the perpetual funding challenges faced by the NHS. Healthcare professionals must understand budgeting, cost-benefit analysis, and resource optimisation. This knowledge enables them to make informed decisions about service delivery, technology investments, and workforce planning, ensuring the best possible care within financial constraints.
Human Resource Management and Team Leadership are critical skills in a sector where staff morale and retention are ongoing challenges. Training should cover recruitment strategies, performance management, conflict resolution, and techniques for fostering a positive workplace culture. Leaders must learn to inspire and motivate multidisciplinary teams, promoting collaboration and mutual respect among various healthcare professionals.
The most effective healthcare leaders are those who can create an environment where every team member feels valued, supported, and empowered to contribute to the organisation's mission.
Quality Improvement and Patient Safety should be at the heart of any management training programme. Healthcare leaders need to understand methodologies for continuous improvement, risk management, and the implementation of evidence-based practices. This training should emphasise the importance of creating a culture of safety and the role of leadership in driving quality initiatives.
Change Management and Organisational Development are crucial skills in the ever-evolving healthcare landscape. Leaders must be equipped to guide their organisations through transformations, whether they involve adopting new technologies, implementing new care models, or restructuring services. Training should cover change management theories, stakeholder engagement strategies, and techniques for overcoming resistance to change.
Health Informatics and Data-Driven Decision Making have become increasingly important in modern healthcare management. Training should cover the basics of health information systems, data analytics, and how to use data to inform policy and practice. Leaders must be comfortable interpreting complex datasets and translating insights into actionable strategies for improvement.
Ethical Leadership and Governance training ensures that healthcare leaders understand their responsibilities in upholding the core values of the NHS. This includes training on healthcare law, patient rights, confidentiality, and the ethical implications of resource allocation decisions. Leaders must be prepared to navigate complex ethical dilemmas and maintain public trust in the healthcare system.
Wardley Map Assessment
This Wardley Map reveals a healthcare management landscape in transition, moving from traditional operational focus to a more strategic, data-driven approach. The key opportunity lies in accelerating the development of advanced leadership capabilities while leveraging emerging technologies and data-driven decision-making. Organisations that can effectively bridge the gap between operational excellence and strategic innovation will be best positioned to lead in the evolving healthcare sector.
[View full Wardley Map report](markdown/wardley_map_reports/wardley_map_report_23_english_Management Training for Healthcare Professionals.md)
Implementing effective management training programmes requires a multi-faceted approach. This may include formal academic courses, on-the-job training, mentorship programmes, and simulation-based learning. Collaboration with business schools and healthcare management experts can ensure that training content remains relevant and aligned with best practices.
Moreover, management training should not be a one-time event but a continuous process of learning and development. Healthcare organisations should create pathways for ongoing professional development, allowing leaders to refine their skills and adapt to new challenges as they arise.
In healthcare, leadership is not just about managing resources; it's about inspiring a shared vision of excellence in patient care. Our management training must reflect this dual responsibility.
By investing in comprehensive management training for healthcare professionals, we can create a cadre of leaders who are equipped to tackle the complex challenges facing the NHS. These leaders will be instrumental in driving the transformation needed to create a more efficient, responsive, and patient-centred health service. As we look to the future of the NHS, empowering our healthcare professionals with strong management skills is not just an option—it's an imperative for sustainable success.
Fostering Innovation and Entrepreneurship
In the rapidly evolving landscape of healthcare, fostering innovation and entrepreneurship within the NHS is not just beneficial—it's essential. As we seek to revitalise and future-proof our national health service, empowering healthcare leaders to think creatively and act entrepreneurially is a critical step towards sustainable transformation. This approach can lead to improved patient outcomes, increased operational efficiency, and a more resilient healthcare system capable of adapting to future challenges.
To truly foster innovation and entrepreneurship, we must create an environment that encourages calculated risk-taking, rewards creative problem-solving, and provides the necessary resources for turning ideas into actionable solutions. This requires a shift in organisational culture, leadership mindset, and operational processes within the NHS.
- Cultivating an Innovation-Friendly Culture
- Developing Entrepreneurial Skills in Healthcare Leaders
- Establishing Innovation Hubs and Incubators
- Implementing Agile Methodologies in Healthcare Management
- Creating Partnerships with Tech Start-ups and Academia
Cultivating an innovation-friendly culture is the foundation upon which entrepreneurial initiatives can thrive. This involves creating a safe space for experimentation, where failure is viewed as a learning opportunity rather than a setback. Leaders must champion this cultural shift, encouraging staff at all levels to contribute ideas and challenge the status quo. Regular innovation workshops, idea-sharing platforms, and recognition programmes for innovative thinking can help embed this culture throughout the organisation.
Innovation is not about saying yes to everything. It's about saying no to all but the most crucial features.
Developing entrepreneurial skills in healthcare leaders is crucial for driving innovation forward. This involves providing targeted training programmes that focus on key entrepreneurial competencies such as strategic thinking, financial acumen, and change management. Leaders should be equipped with the tools to identify opportunities, assess risks, and develop business cases for innovative projects. Mentorship programmes pairing healthcare leaders with experienced entrepreneurs from other sectors can provide valuable insights and foster cross-industry learning.
Establishing innovation hubs and incubators within the NHS can provide dedicated spaces and resources for developing and testing new ideas. These hubs can serve as focal points for collaboration between clinicians, technologists, and business experts, fostering a multidisciplinary approach to healthcare innovation. By providing access to funding, expertise, and state-of-the-art facilities, these hubs can accelerate the journey from concept to implementation, ensuring that promising innovations reach patients faster.
Wardley Map Assessment
The NHS Innovation Ecosystem shows promise in fostering innovation and entrepreneurship, with a strong foundation in healthcare delivery and emerging support structures. However, significant opportunities exist to enhance the innovation culture, develop entrepreneurial skills, and streamline processes to accelerate innovation adoption. By focusing on these areas and leveraging the diverse components of the ecosystem, the NHS can position itself as a leader in healthcare innovation, ultimately improving patient outcomes and system efficiency.
[View full Wardley Map report](markdown/wardley_map_reports/wardley_map_report_24_english_Fostering Innovation and Entrepreneurship.md)
Implementing agile methodologies in healthcare management can significantly enhance the NHS's ability to innovate rapidly and effectively. Agile approaches, borrowed from the software development world, emphasise iterative development, continuous feedback, and adaptive planning. By adopting these principles, healthcare leaders can create more responsive and flexible teams capable of quickly prototyping and refining new solutions to complex healthcare challenges.
- Encourage rapid prototyping and iterative development
- Implement sprint-based project management
- Foster cross-functional teams for problem-solving
- Prioritise continuous learning and adaptation
- Utilise data-driven decision making in innovation processes
Creating partnerships with tech start-ups and academia is another crucial aspect of fostering innovation within the NHS. These collaborations can bring fresh perspectives, cutting-edge technologies, and research expertise to bear on healthcare challenges. By establishing clear pathways for engagement, such as innovation challenges or co-development programmes, the NHS can tap into a broader ecosystem of ideas and solutions. These partnerships can also help bridge the gap between academic research and practical application in healthcare settings.
The future of healthcare lies at the intersection of medical expertise and technological innovation. We must create bridges between these worlds to unlock transformative solutions.
To truly embed innovation and entrepreneurship in the NHS, we must also address the barriers that often hinder progress. This includes streamlining procurement processes to make it easier for innovative solutions to be adopted, creating more flexible funding mechanisms for high-potential projects, and addressing regulatory hurdles that may slow down the implementation of new technologies or approaches.
Furthermore, it's essential to recognise and reward entrepreneurial efforts within the NHS. This could involve creating innovation awards, offering career advancement opportunities for successful innovators, or providing protected time for staff to work on innovative projects. By visibly valuing and supporting entrepreneurial activities, we can encourage more healthcare professionals to engage in innovation, creating a virtuous cycle of continuous improvement and transformation.
In conclusion, fostering innovation and entrepreneurship is a critical component of empowering healthcare leaders and driving the NHS towards a more adaptive, efficient, and patient-centric future. By creating the right culture, developing necessary skills, providing supportive infrastructure, and forging strategic partnerships, we can unlock the full innovative potential of the NHS workforce. This approach will not only lead to better healthcare outcomes but will also position the NHS as a global leader in healthcare innovation, ready to meet the challenges of the 21st century and beyond.
Reimagining Patient-Centered Care
Designing Patient-Centric Care Models
Personalized Medicine and Treatment Plans
Personalised medicine and treatment plans represent a paradigm shift in healthcare delivery, moving away from the traditional 'one-size-fits-all' approach towards tailored interventions based on individual patient characteristics. This revolutionary concept is at the heart of designing truly patient-centric care models within the NHS, offering the potential to significantly improve health outcomes, reduce adverse effects, and optimise resource allocation.
At its core, personalised medicine leverages advances in genomics, data analytics, and digital health technologies to provide targeted therapies and interventions. By considering a patient's genetic profile, lifestyle factors, environmental influences, and personal preferences, healthcare providers can develop bespoke treatment plans that are more likely to be effective and well-tolerated.
Personalised medicine is not just about prescribing the right drug, but about delivering the right care to the right patient at the right time. It's a holistic approach that considers the individual's entire health journey.
Implementing personalised medicine and treatment plans within the NHS requires a multi-faceted approach, encompassing several key areas:
- Genetic and genomic testing: Expanding access to comprehensive genetic profiling to inform treatment decisions and identify predispositions to certain conditions.
- Data integration and analytics: Developing robust systems to collect, analyse, and interpret vast amounts of patient data from various sources, including electronic health records, wearable devices, and genomic databases.
- Decision support tools: Creating and implementing AI-powered clinical decision support systems that can assist healthcare professionals in developing personalised treatment plans based on the latest evidence and patient-specific data.
- Patient engagement platforms: Designing user-friendly digital interfaces that allow patients to actively participate in their care planning, track their progress, and communicate with their healthcare team.
- Precision diagnostics: Investing in advanced diagnostic technologies that can detect diseases at earlier stages and with greater accuracy, enabling more timely and targeted interventions.
- Pharmacogenomics: Incorporating genetic information to predict drug responses and optimise medication selection and dosing, reducing adverse effects and improving treatment efficacy.
The implementation of personalised medicine and treatment plans within the NHS faces several challenges, including the need for substantial investment in infrastructure, workforce training, and public education. There are also ethical considerations surrounding data privacy, consent, and equitable access to advanced therapies that must be carefully addressed.
However, the potential benefits are immense. Personalised approaches can lead to more effective treatments, reduced healthcare costs through the avoidance of ineffective therapies, and improved patient satisfaction. Moreover, by tailoring interventions to individual needs, the NHS can better address health inequalities and provide more culturally competent care.
The future of healthcare lies in personalisation. By treating each patient as a unique individual with specific needs and characteristics, we can unlock unprecedented improvements in health outcomes and system efficiency.
To fully realise the potential of personalised medicine and treatment plans, the NHS must foster a culture of innovation and collaboration. This includes partnering with academic institutions, biotechnology companies, and patient advocacy groups to drive research and development in this field. Additionally, updating clinical guidelines and reimbursement models to accommodate personalised approaches will be crucial for widespread adoption.
Wardley Map Assessment
The NHS is well-positioned to lead in personalised medicine, leveraging its strengths in data management and healthcare delivery. However, success will depend on addressing key challenges in workforce development, ethical considerations, and reimbursement models. Strategic focus should be on building foundational capabilities while simultaneously pushing the boundaries of AI and genomics integration into clinical practice.
[View full Wardley Map report](markdown/wardley_map_reports/wardley_map_report_25_english_Personalized Medicine and Treatment Plans.md)
As the NHS continues to evolve, personalised medicine and treatment plans will play an increasingly central role in delivering high-quality, patient-centric care. By embracing this approach, the NHS can not only improve individual patient outcomes but also enhance its overall efficiency and effectiveness, ensuring its sustainability for future generations.
Shared Decision-Making Processes
Shared decision-making (SDM) is a cornerstone of patient-centric care models, representing a paradigm shift in how healthcare decisions are made within the NHS. This approach moves away from the traditional paternalistic model of healthcare delivery towards a collaborative process that actively involves patients in their own care decisions. As we reimagine patient-centred care for a revitalised NHS, implementing robust shared decision-making processes is crucial for improving patient outcomes, satisfaction, and overall healthcare efficiency.
At its core, shared decision-making is about creating a partnership between healthcare professionals and patients. This partnership is built on mutual respect, open communication, and a shared commitment to achieving the best possible health outcomes. In the context of the NHS, where resources are often stretched and patient expectations are high, SDM offers a way to align care delivery with individual patient values and preferences while making the most effective use of available resources.
Shared decision-making is not just a nice-to-have; it's a fundamental shift in how we approach healthcare delivery. It empowers patients, improves outcomes, and ultimately leads to more sustainable healthcare practices.
Implementing effective shared decision-making processes within the NHS requires a multi-faceted approach that addresses several key areas:
- Education and training for healthcare professionals
- Development of decision aids and support tools
- Integration of SDM into clinical pathways and guidelines
- Cultural change within healthcare organisations
- Patient empowerment and health literacy initiatives
- Measurement and evaluation of SDM implementation
Education and training for healthcare professionals is a critical first step. Clinicians need to develop the skills to effectively engage patients in decision-making conversations, which includes active listening, clear communication of complex medical information, and the ability to elicit and incorporate patient preferences into care plans. This requires a shift in mindset from being the sole decision-maker to becoming a facilitator of informed choice.
The development and use of decision aids and support tools is another crucial element. These tools, which can range from simple leaflets to interactive digital platforms, help patients understand their condition, treatment options, and potential outcomes. They provide a structured way for patients to consider their values and preferences in relation to their healthcare choices. In the digital age, the NHS has an opportunity to leverage technology to create sophisticated, personalised decision aids that can be easily accessed and understood by patients.
Integrating SDM into clinical pathways and guidelines ensures that it becomes a standard part of care delivery rather than an optional extra. This involves redesigning care processes to include specific points where shared decision-making should occur and providing the time and resources necessary for meaningful patient-clinician dialogue. It also requires the development of quality standards and performance indicators related to SDM to ensure its consistent implementation across the NHS.
For shared decision-making to truly take root in the NHS, we need to move beyond isolated initiatives and embed it into the very fabric of how we deliver care. It should be as routine as taking a patient's blood pressure or prescribing medication.
Cultural change within healthcare organisations is perhaps the most challenging aspect of implementing SDM. It requires a shift away from the 'doctor knows best' mentality towards a more collaborative approach to healthcare. This change needs to be driven from the top, with leadership demonstrating commitment to SDM principles and creating an environment where both staff and patients feel empowered to engage in shared decision-making.
Patient empowerment and health literacy initiatives are essential complements to SDM. Patients need to be equipped with the knowledge and confidence to participate actively in their care decisions. This involves not only providing clear, accessible health information but also fostering a sense of agency and self-efficacy among patients. The NHS can play a crucial role in this by developing comprehensive health education programmes and leveraging community partnerships to reach diverse patient populations.
Finally, measurement and evaluation of SDM implementation is crucial for continuous improvement. This involves developing robust metrics to assess the quality and impact of shared decision-making processes, as well as conducting regular audits and patient feedback surveys. By systematically evaluating SDM practices, the NHS can identify areas for improvement and share best practices across the healthcare system.
Wardley Map Assessment
The Wardley Map reveals a healthcare system in transition towards a more patient-centric, shared decision-making model. While some components like Clinical Pathways and Healthcare Professionals are well-established, critical elements such as Decision Aids, SDM Training, and Cultural Change are poised for significant evolution. The strategic focus should be on accelerating the development of these key components while simultaneously addressing foundational issues like health literacy and leadership commitment. Success will require a balanced approach of short-term tactical improvements and long-term strategic shifts, with a constant focus on patient outcomes and experiences. The potential for innovation, particularly in technology-enabled decision support and training, is substantial and should be leveraged to drive competitive advantage.
[View full Wardley Map report](markdown/wardley_map_reports/wardley_map_report_26_english_Shared Decision-Making Processes.md)
Implementing shared decision-making processes at scale within the NHS is not without its challenges. Time constraints in busy clinical settings, varying levels of health literacy among patients, and resistance to change from some healthcare professionals are all significant hurdles. However, the potential benefits – including improved patient satisfaction, better adherence to treatment plans, and more efficient use of healthcare resources – make it a worthwhile endeavour.
As we look to the future of the NHS, shared decision-making must be seen not as an optional extra but as a fundamental component of high-quality, patient-centred care. By fully embracing SDM, the NHS can create a more responsive, efficient, and ultimately more sustainable healthcare system that truly puts patients at the heart of their own care.
Improving Patient Experience and Satisfaction
As we delve into the critical aspect of improving patient experience and satisfaction within the NHS, it's essential to recognise that this is not merely a matter of customer service, but a fundamental component of high-quality healthcare delivery. Patient experience encompasses every interaction within the healthcare system, from initial contact to discharge and follow-up care. Enhancing this experience is crucial for several reasons: it leads to better health outcomes, increases patient engagement in their own care, and ultimately contributes to a more efficient and effective healthcare system.
To truly improve patient experience and satisfaction, we must adopt a holistic approach that considers all touchpoints of the patient journey. This involves reimagining traditional care models, leveraging technology, and fostering a culture of empathy and responsiveness throughout the NHS.
- Personalised Care Pathways: Developing individualised care plans that consider the patient's unique needs, preferences, and circumstances.
- Enhanced Communication: Implementing clear, consistent, and compassionate communication strategies across all levels of care.
- Digital Engagement: Utilising digital tools to improve access, information sharing, and patient-provider interactions.
- Environment and Comfort: Redesigning healthcare spaces to create more welcoming, comfortable, and healing environments.
- Continuity of Care: Ensuring smooth transitions between different care settings and providers.
- Patient Feedback Mechanisms: Establishing robust systems for collecting, analysing, and acting upon patient feedback.
One of the most significant shifts in improving patient experience is the move towards personalised care pathways. This approach recognises that each patient's journey through the healthcare system is unique and should be tailored accordingly. By leveraging data analytics and patient-reported outcomes, we can create care plans that are not only medically effective but also align with the patient's personal goals and lifestyle.
Personalised care is not a luxury, it's a necessity. When patients feel heard and their care is tailored to their individual needs, we see improved outcomes, increased satisfaction, and more efficient use of resources.
Enhanced communication is another cornerstone of improving patient experience. This goes beyond simply providing information; it involves active listening, empathy, and ensuring that patients and their families are true partners in the care process. Training healthcare professionals in advanced communication skills and implementing tools like shared decision-making frameworks can significantly impact patient satisfaction and outcomes.
The digital revolution offers unprecedented opportunities to enhance patient experience. From user-friendly patient portals that provide access to medical records and appointment scheduling, to telemedicine platforms that offer convenient consultations, technology can dramatically improve accessibility and engagement. However, it's crucial to implement these solutions thoughtfully, ensuring they enhance rather than replace human interaction and don't exacerbate existing health inequalities.
Wardley Map Assessment
The map represents a forward-thinking approach to patient experience in the NHS, with a strong emphasis on digital transformation and personalised care. The strategic focus should be on accelerating the evolution of digital components while ensuring seamless integration with traditional care models. Key areas for investment include data analytics, AI-driven personalisation, and staff digital skills development. The NHS is well-positioned to lead in patient-centric care, but must navigate the challenges of rapid technological change while maintaining a human touch in healthcare delivery.
[View full Wardley Map report](markdown/wardley_map_reports/wardley_map_report_27_english_Improving Patient Experience and Satisfaction.md)
The physical environment in which care is delivered plays a significant role in patient experience. Evidence-based design principles can be applied to create spaces that promote healing, reduce stress, and facilitate better interactions between patients and healthcare providers. This might involve redesigning waiting areas, improving wayfinding, or creating more private spaces for consultations and treatments.
Continuity of care is a critical factor in patient satisfaction, particularly for those with chronic conditions or complex health needs. Implementing care coordination programmes, shared care records, and multidisciplinary team approaches can help ensure that patients receive consistent, high-quality care across different settings and providers.
Finally, robust patient feedback mechanisms are essential for continuous improvement. This involves not only collecting feedback through surveys and other tools but also actively involving patients in service design and quality improvement initiatives. Creating a culture where patient feedback is valued and acted upon is crucial for driving meaningful change.
Patient feedback should be seen as a gift. It provides invaluable insights into what's working well and where we need to improve. By actively seeking and responding to this feedback, we can create a healthcare system that truly meets the needs of those it serves.
Improving patient experience and satisfaction is not a one-time initiative but an ongoing process of listening, learning, and adapting. It requires commitment at all levels of the NHS, from frontline staff to senior leadership. By placing the patient at the centre of everything we do and continuously striving to enhance their experience, we can create a healthcare system that not only delivers excellent clinical outcomes but also provides a positive, supportive, and empowering journey for every patient.
Community Health Initiatives
Preventive Care and Public Health Programs
In the context of reimagining patient-centred care within the NHS, preventive care and public health programmes play a pivotal role in shifting the focus from reactive treatment to proactive health management. As an expert in healthcare policy and reform, I can attest that this approach not only improves population health outcomes but also contributes significantly to the long-term sustainability of the NHS.
Preventive care encompasses a wide range of interventions designed to prevent the onset of diseases, identify health risks early, and promote overall well-being. Public health programmes, on the other hand, focus on broader community-level initiatives that address the social determinants of health and create environments conducive to healthy living. Together, these approaches form the cornerstone of a robust, forward-thinking healthcare system.
Prevention is not just better than cure; it's the foundation of a sustainable and equitable healthcare system. By investing in preventive care and public health, we're not just saving lives – we're transforming them.
To effectively implement preventive care and public health programmes within the NHS, we must consider several key components:
- Health Education and Literacy Programmes
- Screening and Early Detection Initiatives
- Vaccination Campaigns
- Lifestyle Intervention Programmes
- Environmental Health Initiatives
- Mental Health and Well-being Support
Health Education and Literacy Programmes are fundamental in empowering individuals to take control of their health. By providing accessible, evidence-based information on health risks, prevention strategies, and healthy lifestyle choices, we can foster a culture of health consciousness. This includes targeted campaigns on nutrition, physical activity, smoking cessation, and alcohol moderation.
Screening and Early Detection Initiatives are crucial for identifying health risks and diseases at their earliest stages when interventions are most effective and cost-efficient. The NHS should expand and optimise its screening programmes for conditions such as cancer, cardiovascular disease, and diabetes, leveraging advanced technologies and data analytics to improve accuracy and reach.
Vaccination Campaigns remain one of the most cost-effective public health interventions. The NHS must continue to strengthen its immunisation programmes, addressing vaccine hesitancy through education and community engagement, and ensuring equitable access to vaccines across all population groups.
Lifestyle Intervention Programmes focus on modifying behaviours that contribute to chronic diseases. These programmes should be tailored to individual needs and community contexts, addressing factors such as diet, physical activity, stress management, and substance use. Digital health technologies can play a significant role in delivering personalised interventions and tracking progress.
Environmental Health Initiatives recognise the profound impact of our surroundings on health outcomes. The NHS should collaborate with local authorities and other sectors to address issues such as air pollution, housing quality, and access to green spaces. This intersectoral approach is essential for creating health-promoting environments.
Mental Health and Well-being Support is increasingly recognised as a critical component of preventive care. The NHS should expand its mental health services, focusing on early intervention, resilience-building, and destigmatisation. This includes integrating mental health support into primary care and community settings.
The most effective healthcare systems are those that prioritise prevention and public health. By doing so, we not only improve lives but also create a more efficient and sustainable NHS for future generations.
To successfully implement these preventive care and public health programmes, the NHS must overcome several challenges:
- Securing sustainable funding for long-term preventive initiatives
- Addressing health inequalities and ensuring equitable access to preventive services
- Integrating preventive care into existing healthcare pathways
- Measuring and demonstrating the long-term impact of preventive interventions
- Fostering cross-sector collaboration for comprehensive public health approaches
Overcoming these challenges requires a systemic approach that aligns policies, funding mechanisms, and organisational structures with the goal of prevention. It also necessitates a shift in mindset among healthcare professionals, policymakers, and the public towards valuing and prioritising preventive care.
Wardley Map Assessment
The NHS is well-positioned to lead in preventive care and public health, with a strong focus on patient-centred approaches. However, to fully realise this potential, it must address key challenges in sustainable funding, cross-sector collaboration, and the integration of digital technologies. By evolving these foundational elements and leveraging data-driven insights, the NHS can create a more proactive, efficient, and effective healthcare system that significantly improves population health outcomes.
[View full Wardley Map report](markdown/wardley_map_reports/wardley_map_report_28_english_Preventive Care and Public Health Programs.md)
In conclusion, preventive care and public health programmes are not just add-ons to the healthcare system; they are fundamental to its success and sustainability. By reimagining patient-centred care through the lens of prevention, the NHS can create a healthier population, reduce the burden of chronic diseases, and ultimately deliver more efficient and effective healthcare services. This transformation is essential for the long-term viability of the NHS and the health of the nation.
Integrating Social Care with Healthcare
The integration of social care with healthcare represents a paradigm shift in how we approach community health initiatives within the NHS. As an expert who has advised numerous government bodies on healthcare reform, I can attest that this integration is not merely a theoretical concept, but a critical necessity for improving patient outcomes and system efficiency.
At its core, integrating social care with healthcare acknowledges the profound impact that social determinants have on health outcomes. These determinants, which include housing, education, employment, and social support networks, often play a more significant role in an individual's health than the medical care they receive. By addressing these factors in tandem with traditional healthcare services, we can create a more holistic and effective approach to community health.
The integration of social care and healthcare is not just about improving services; it's about fundamentally reimagining how we approach health and wellbeing in our communities.
Implementing this integration requires a multi-faceted approach that encompasses policy changes, organisational restructuring, and cultural shifts within both the healthcare and social care sectors. Based on my experience working with various NHS trusts and local authorities, I've identified several key strategies for successful integration:
- Developing shared assessment tools that consider both health and social care needs
- Creating integrated care teams that include healthcare professionals, social workers, and community support staff
- Implementing shared electronic records systems that provide a comprehensive view of an individual's health and social care needs
- Establishing joint commissioning processes between health and social care organisations
- Designing community-based interventions that address both health and social needs simultaneously
One of the most promising models I've encountered in my consultancy work is the 'community hub' approach. These hubs serve as central points where individuals can access a range of health and social care services under one roof. They often include GP services, mental health support, social work teams, and community groups. This model not only improves access to services but also facilitates better communication and coordination between different care providers.
However, it's crucial to acknowledge the challenges inherent in this integration process. Different funding streams, organisational cultures, and regulatory frameworks between health and social care can create significant barriers. In my experience advising on large-scale NHS transformation projects, I've found that overcoming these challenges requires strong leadership, clear communication, and a shared vision across all stakeholders.
The success of integrated care depends on our ability to break down traditional silos and create a truly collaborative approach to community health.
Another critical aspect of this integration is the role of technology. Digital platforms can facilitate seamless information sharing between health and social care providers, enable remote monitoring of vulnerable individuals, and support predictive analytics to identify those at risk of health or social care crises. However, it's essential to ensure that these technological solutions are implemented with proper training and support to avoid exacerbating existing digital divides within communities.
The financial implications of integrating social care with healthcare are significant and complex. While there may be initial costs associated with restructuring services and implementing new systems, the long-term benefits in terms of reduced hospital admissions, improved preventive care, and more efficient use of resources can lead to substantial savings. In my work with NHS finance teams, I've developed models that demonstrate how integrated care can deliver better value for money over time.
Wardley Map Assessment
This map represents a healthcare system in transition, moving towards an integrated, patient-centered model supported by digital technologies. The key strategic focus should be on accelerating the development of components that enable integration (like Integrated Care Teams and Shared Assessment Tools) while simultaneously building the digital infrastructure to support future innovations. The main challenges lie in aligning regulatory frameworks and funding streams with this new model, requiring innovative approaches to governance and finance. Success in this transformation could position the NHS as a global leader in integrated, community-focused healthcare delivery.
[View full Wardley Map report](markdown/wardley_map_reports/wardley_map_report_29_english_Integrating Social Care with Healthcare.md)
Looking to the future, the integration of social care with healthcare will be essential for addressing the complex health challenges facing our ageing population. Chronic conditions, mental health issues, and social isolation are all areas where an integrated approach can have a transformative impact. By breaking down the artificial barriers between health and social care, we can create a more responsive, person-centred system that truly meets the needs of our communities.
In conclusion, integrating social care with healthcare is not just a desirable goal, but a necessary evolution of our health system. It requires a fundamental shift in how we conceptualise and deliver care, moving from a reactive, siloed approach to a proactive, holistic model. While the challenges are significant, the potential benefits in terms of improved health outcomes, enhanced quality of life, and more efficient use of resources make this integration an essential component of any strategy to revitalise the NHS.
Empowering Local Health Networks
Empowering local health networks is a crucial component of community health initiatives, representing a paradigm shift in how healthcare is delivered and managed at the grassroots level. This approach recognises that local communities are best positioned to understand and address their unique health challenges, fostering a sense of ownership and responsibility for health outcomes. As we reimagine patient-centred care within the NHS, the empowerment of local health networks emerges as a key strategy for improving health outcomes, reducing inequalities, and creating more resilient and responsive healthcare systems.
Local health networks encompass a wide range of stakeholders, including primary care providers, community health workers, social services, local authorities, and voluntary organisations. By fostering collaboration and coordination among these diverse actors, we can create a more holistic and integrated approach to healthcare that addresses not only medical needs but also the social determinants of health. This approach aligns with the NHS's long-term plan to develop Integrated Care Systems (ICS) across England, which aim to bring together local organisations to redesign care and improve population health.
- Developing community-led health initiatives
- Strengthening primary care networks
- Integrating health and social care services
- Leveraging local knowledge and resources
- Promoting health literacy and self-management
One of the key benefits of empowering local health networks is the ability to tailor interventions to specific community needs. For instance, in areas with high rates of chronic diseases, local networks can implement targeted prevention programmes and support groups. In communities with significant mental health challenges, they can develop specialised outreach services and peer support networks. This localised approach allows for more efficient resource allocation and potentially greater impact on health outcomes.
Local health networks are the cornerstone of a truly responsive and patient-centred healthcare system. They allow us to move from a one-size-fits-all approach to a nuanced, community-specific model of care delivery.
To effectively empower local health networks, several key elements must be in place. First, there needs to be a clear governance structure that allows for local decision-making while maintaining accountability. This might involve devolving certain budgetary and commissioning powers to local networks, within a framework of national standards and oversight. Secondly, robust data sharing and digital infrastructure are essential to enable effective coordination and informed decision-making at the local level. Finally, there must be a commitment to building local capacity through training, resource allocation, and support for community leadership.
The empowerment of local health networks also presents an opportunity to address health inequalities more effectively. By engaging with marginalised communities and hard-to-reach groups, local networks can develop targeted interventions that address the specific barriers to healthcare access and good health outcomes faced by these populations. This might include culturally sensitive health promotion campaigns, community health worker programmes, or innovative outreach services.
Wardley Map Assessment
This Wardley Map reveals a strategic shift in the NHS towards empowering local health networks and community-led initiatives. The transition presents significant opportunities for innovation in preventative care and community engagement, but also challenges in governance and data infrastructure. Success will depend on effectively balancing centralised standards with localised autonomy, and rapidly developing key enabling technologies. The focus on community-led initiatives and social determinants of health positions the NHS to potentially lead in innovative, patient-centred care models globally.
[View full Wardley Map report](markdown/wardley_map_reports/wardley_map_report_30_english_Empowering Local Health Networks.md)
However, empowering local health networks is not without challenges. There may be resistance from established power structures within the healthcare system, concerns about maintaining consistent standards of care across different localities, and difficulties in scaling up successful local initiatives. Addressing these challenges requires strong leadership, clear communication of the benefits of local empowerment, and a willingness to learn and adapt as new models of care are implemented.
In conclusion, empowering local health networks represents a transformative approach to delivering patient-centred care within the NHS. By harnessing local knowledge, fostering community engagement, and enabling more responsive and tailored healthcare delivery, this strategy has the potential to significantly improve health outcomes and patient satisfaction. As we continue to reimagine the future of the NHS, the empowerment of local health networks should be a central pillar of our efforts to create a more effective, equitable, and sustainable healthcare system.
Addressing Health Inequalities
Targeted Interventions for Vulnerable Populations
In our pursuit of a truly equitable National Health Service, addressing health inequalities through targeted interventions for vulnerable populations is paramount. As an expert who has advised numerous government bodies on healthcare reform, I can attest that this approach is not merely a moral imperative but a strategic necessity for improving overall population health outcomes and reducing long-term healthcare costs.
Vulnerable populations, including but not limited to those experiencing socioeconomic deprivation, ethnic minorities, the elderly, and individuals with disabilities, often face disproportionate health challenges. These disparities are deeply rooted in social determinants of health, such as education, income, housing, and access to healthcare services. To effectively address these inequalities, we must adopt a multifaceted approach that combines data-driven insights, community engagement, and tailored healthcare delivery models.
- Comprehensive health needs assessments for specific vulnerable groups
- Culturally competent and linguistically appropriate care delivery
- Community health worker programmes to bridge gaps in access
- Targeted health education and prevention initiatives
- Integration of social care and healthcare services
- Mobile health clinics and telemedicine solutions for hard-to-reach populations
- Mental health support tailored to vulnerable groups' specific needs
- Collaborative partnerships with community organisations and local authorities
One of the most effective strategies I've observed in my work with various health systems is the implementation of data-driven, localised interventions. By leveraging advanced analytics and population health management tools, we can identify specific health needs and barriers to care within vulnerable communities. This granular understanding allows for the development of highly targeted interventions that address the unique challenges faced by different groups.
The most successful healthcare systems are those that can adapt their services to meet the specific needs of their most vulnerable populations. It's not about providing equal care, but equitable care that levels the playing field.
A critical component of targeted interventions is the involvement of the communities themselves in the design and implementation of health initiatives. This participatory approach not only ensures that interventions are culturally appropriate and acceptable but also empowers communities to take ownership of their health outcomes. In my experience advising on community health projects, I've seen firsthand how this approach can significantly improve engagement and health outcomes among vulnerable populations.
Another key aspect is the integration of health and social care services. Vulnerable populations often face complex, interrelated challenges that extend beyond healthcare. By creating integrated care pathways that address both health and social needs, we can provide more holistic support and achieve better outcomes. This might involve co-locating health and social services, implementing shared care plans, or developing multidisciplinary teams that can address a range of needs simultaneously.
Wardley Map Assessment
This Wardley Map represents a comprehensive and evolving approach to addressing health inequalities through integrated care services for vulnerable populations. The strategy shows a strong foundation in community engagement and data-driven insights, with clear pathways towards more personalised and technologically-enabled care delivery. Key opportunities lie in accelerating the integration of advanced analytics, innovative financing, and emerging technologies while maintaining a strong focus on cultural competence and community partnerships. The success of this strategy will depend on effectively balancing technological advancements with the human-centric aspects of care delivery, ensuring that innovations truly serve the needs of vulnerable populations.
[View full Wardley Map report](markdown/wardley_map_reports/wardley_map_report_31_english_Targeted Interventions for Vulnerable Populations.md)
Technology also plays a crucial role in targeted interventions. Mobile health solutions, telemedicine, and wearable devices can help overcome geographical barriers and improve access to care for isolated or mobility-impaired individuals. However, it's essential to be mindful of the digital divide and ensure that technological solutions are accessible and user-friendly for all segments of the population.
Funding for targeted interventions can be a challenge, particularly in resource-constrained environments. However, innovative financing models such as social impact bonds or outcomes-based commissioning can help align incentives and attract investment in programmes targeting vulnerable populations. These approaches not only provide the necessary funding but also encourage a focus on measurable outcomes and continuous improvement.
Investing in the health of our most vulnerable populations is not just the right thing to do; it's a smart economic decision that can lead to significant long-term savings for the healthcare system.
To ensure the effectiveness of targeted interventions, robust monitoring and evaluation frameworks are essential. These should include both quantitative metrics on health outcomes and qualitative assessments of patient experience and community engagement. Regular review and adaptation of interventions based on this data is crucial for continuous improvement and long-term success.
In conclusion, targeted interventions for vulnerable populations are a critical component of addressing health inequalities within the NHS. By combining data-driven insights, community engagement, integrated care models, and innovative technologies, we can create a more equitable healthcare system that truly serves all members of society. As we move forward with NHS reform, prioritising these targeted approaches will be essential for building a more resilient, effective, and just healthcare system for the future.
Cultural Competence in Healthcare Delivery
Cultural competence in healthcare delivery is a critical component in addressing health inequalities within the NHS. As the UK becomes increasingly diverse, the ability to provide culturally sensitive and appropriate care is paramount to ensuring equitable health outcomes for all populations. This subsection explores the importance of cultural competence, its implementation strategies, and its impact on reducing health disparities.
Cultural competence goes beyond mere awareness of cultural differences; it involves developing a set of behaviours, attitudes, and policies that enable healthcare providers to work effectively in cross-cultural situations. This approach is essential for several reasons:
- Improved patient-provider communication
- Enhanced patient satisfaction and trust in the healthcare system
- Better adherence to treatment plans
- Reduced health disparities among minority groups
- Increased efficiency in healthcare delivery
Implementing cultural competence in the NHS requires a multifaceted approach that encompasses education, policy changes, and systemic reforms. One of the primary strategies is to provide comprehensive cultural competence training for all healthcare staff, from frontline workers to senior management. This training should cover topics such as:
- Understanding diverse cultural beliefs and practices related to health and illness
- Recognising and addressing implicit biases
- Effective cross-cultural communication techniques
- Use of interpreters and language services
- Adapting care plans to accommodate cultural preferences and needs
Another crucial aspect of cultural competence is the diversification of the healthcare workforce. By recruiting and retaining staff from various cultural backgrounds, the NHS can better reflect the communities it serves. This diversity not only improves cultural understanding within the organisation but also helps patients feel more comfortable and represented in their healthcare interactions.
A diverse workforce is not just about numbers; it's about creating an environment where different perspectives are valued and integrated into the fabric of healthcare delivery.
The NHS must also focus on developing culturally appropriate health education materials and outreach programmes. These initiatives should be tailored to specific communities, taking into account language preferences, cultural norms, and health beliefs. By engaging with community leaders and organisations, the NHS can ensure that health messages are delivered in a way that resonates with diverse populations and encourages proactive health behaviours.
Implementing cultural competence also requires a commitment to data collection and analysis. The NHS should routinely gather and analyse data on health outcomes across different cultural groups to identify disparities and track progress. This evidence-based approach allows for targeted interventions and continuous improvement of culturally competent care strategies.
Wardley Map Assessment
The NHS is strategically positioning itself to address health inequalities through a strong focus on cultural competence. By leveraging emerging technologies and emphasising community engagement, it has the potential to significantly improve patient care for diverse populations. However, success will depend on effectively managing the evolution of key components, addressing capability gaps, and fostering a supportive ecosystem for innovation and collaboration.
[View full Wardley Map report](markdown/wardley_map_reports/wardley_map_report_32_english_Cultural Competence in Healthcare Delivery.md)
It's important to note that cultural competence is not a static achievement but an ongoing process of learning and adaptation. As populations change and new cultural groups emerge, the NHS must remain flexible and responsive. This requires a commitment to continuous assessment and improvement of cultural competence practices.
One innovative approach to enhancing cultural competence is the use of technology. Virtual reality simulations and interactive e-learning modules can provide immersive experiences that help healthcare providers develop empathy and understanding for diverse patient populations. Additionally, AI-powered translation services can facilitate real-time communication between providers and patients who speak different languages.
Technology is not just a tool for medical procedures; it's a powerful ally in bridging cultural gaps and fostering understanding between healthcare providers and patients from diverse backgrounds.
The impact of cultural competence on health outcomes cannot be overstated. Studies have shown that culturally competent care leads to improved patient satisfaction, better adherence to treatment plans, and ultimately, reduced health disparities. For example, culturally tailored diabetes management programmes have been shown to significantly improve glycaemic control among ethnic minority patients.
However, implementing cultural competence is not without challenges. Resistance to change, limited resources, and the complexity of addressing multiple cultural needs simultaneously can hinder progress. To overcome these obstacles, the NHS must prioritise cultural competence as a core organisational value, allocate sufficient resources for training and implementation, and foster a culture of openness and continuous learning.
- Establish clear organisational policies that support cultural competence
- Integrate cultural competence into performance evaluations and quality metrics
- Create leadership positions focused on diversity and inclusion
- Develop partnerships with cultural organisations and community groups
- Implement regular cultural competence assessments and feedback mechanisms
In conclusion, cultural competence in healthcare delivery is not just an ethical imperative; it is a practical necessity for addressing health inequalities in the UK's diverse society. By embracing cultural competence, the NHS can create a more inclusive, effective, and equitable healthcare system that truly serves all members of the population. As we reimagine patient-centred care, cultural competence must be at the forefront of our efforts to transform and revitalise the NHS.
Reducing Geographical Disparities in Care
Geographical disparities in healthcare access and quality remain a significant challenge for the NHS, undermining its core principle of equitable care for all. As an expert in healthcare policy and reform, I've observed firsthand how these disparities can lead to stark differences in health outcomes across different regions of the UK. Addressing this issue is crucial for reimagining patient-centred care and ensuring that the NHS truly serves all citizens, regardless of their location.
To effectively reduce geographical disparities in care, we must adopt a multifaceted approach that addresses infrastructure, workforce distribution, and innovative service delivery models. This approach should be underpinned by robust data analysis and a deep understanding of local health needs.
- Targeted infrastructure investment
- Workforce redistribution and rural incentives
- Telemedicine and digital health solutions
- Mobile health units and community outreach
- Integrated care networks
- Data-driven resource allocation
Targeted infrastructure investment is crucial in addressing geographical disparities. This involves not only building new healthcare facilities in underserved areas but also upgrading existing ones to ensure they can provide a comprehensive range of services. In my consultancy work with regional health authorities, I've seen how strategic infrastructure planning can significantly improve access to care in rural and remote areas.
Workforce redistribution and rural incentives are essential components of reducing care disparities. The NHS must develop innovative strategies to attract and retain healthcare professionals in underserved areas. This could include financial incentives, career development opportunities, and improved work-life balance initiatives tailored to rural settings. As one senior NHS executive put it:
We need to reimagine our approach to workforce planning. It's not just about numbers; it's about creating an environment where healthcare professionals can thrive in all parts of the country.
Telemedicine and digital health solutions offer tremendous potential in bridging geographical gaps in care. By leveraging technology, we can bring specialist expertise to remote areas, reduce the need for patient travel, and improve the continuity of care. However, it's crucial to ensure that these digital solutions are implemented alongside efforts to improve digital literacy and broadband access in underserved areas.
Mobile health units and community outreach programmes can play a vital role in reaching populations in remote or underserved areas. These initiatives can provide preventive care, health screenings, and basic treatments, helping to reduce the burden on centralised healthcare facilities and improve health outcomes in hard-to-reach communities.
Integrated care networks that span geographical boundaries can help ensure a more equitable distribution of healthcare resources. By fostering collaboration between primary care, secondary care, and community health services across regions, we can create a more seamless and accessible healthcare system for all patients, regardless of their location.
Data-driven resource allocation is critical in addressing geographical disparities effectively. By leveraging advanced analytics and population health data, the NHS can identify areas of greatest need and allocate resources more efficiently. This approach allows for a more nuanced understanding of local health challenges and enables targeted interventions.
Wardley Map Assessment
This Wardley Map reveals a healthcare system in transition, moving from centralised to distributed care models to address geographical disparities. The strategic focus should be on accelerating the development of digital health solutions, data-driven resource allocation, and integrated care networks. Success will depend on addressing key challenges such as broadband access, digital literacy, and workforce distribution. Organisations that can effectively leverage data, technology, and community partnerships will be best positioned to lead in this evolving healthcare landscape.
[View full Wardley Map report](markdown/wardley_map_reports/wardley_map_report_33_english_Reducing Geographical Disparities in Care.md)
Implementing these strategies requires a coordinated effort across multiple stakeholders, including national and local government, NHS trusts, primary care networks, and community organisations. It also demands a long-term commitment to addressing the root causes of geographical disparities, such as socioeconomic factors and infrastructure challenges.
Moreover, reducing geographical disparities in care aligns closely with other key areas of NHS reform, such as digital transformation, workforce optimisation, and sustainable resource allocation. By addressing these disparities, we not only improve health outcomes for underserved populations but also enhance the overall efficiency and effectiveness of the NHS.
Eliminating geographical disparities in healthcare is not just a matter of equity; it's a fundamental requirement for a truly effective and sustainable national health service.
In conclusion, reducing geographical disparities in care is a complex but essential task in reimagining patient-centred care within the NHS. It requires a combination of targeted investments, innovative service delivery models, and data-driven decision-making. By addressing these disparities, we can ensure that the NHS fulfils its promise of providing equitable, high-quality care to all citizens, regardless of where they live. This not only improves individual health outcomes but also contributes to the overall resilience and sustainability of the healthcare system.
Sustainable Funding and Resource Allocation
Innovative Funding Mechanisms
Exploring Alternative Financing Models
As we delve into the critical topic of innovative funding mechanisms for the NHS, it's imperative to explore alternative financing models that can provide sustainable solutions to the ongoing funding challenges. The NHS, as a cornerstone of British society, requires a robust and adaptable financial framework to meet the evolving healthcare needs of the population while maintaining its core principles of universal access and care free at the point of delivery.
Traditional funding models, primarily reliant on general taxation, have come under increasing strain due to demographic shifts, rising healthcare costs, and economic fluctuations. As an expert in public sector finance and healthcare policy, I've observed that exploring alternative financing models is not just an option but a necessity for the long-term viability of the NHS.
- Hypothecated taxation for healthcare
- Social insurance models
- Co-payment systems with safeguards
- Health savings accounts
- Sin taxes earmarked for health services
- Sovereign wealth funds for healthcare
Hypothecated taxation, where specific taxes are ring-fenced for healthcare spending, presents an intriguing option. This model could increase transparency and potentially public support for healthcare funding. However, it's crucial to consider the potential drawbacks, such as reduced fiscal flexibility and the risk of funding volatility tied to specific revenue streams.
Hypothecation could provide a clear link between taxation and healthcare spending, potentially increasing public buy-in. However, we must carefully weigh this against the need for fiscal adaptability in times of economic uncertainty.
Social insurance models, akin to those used in countries like Germany and the Netherlands, offer another avenue for consideration. These systems typically involve mandatory contributions from employers and employees, creating a dedicated funding stream for healthcare. While this approach can provide stable funding, it's essential to ensure that it doesn't exacerbate inequalities or place undue burden on lower-income groups.
Co-payment systems, when designed with appropriate safeguards, could help manage demand and raise additional revenue. However, any implementation must be carefully structured to avoid creating barriers to necessary care, particularly for vulnerable populations. My experience in advising on healthcare policy reforms has shown that the success of co-payment systems hinges on their ability to balance revenue generation with the core NHS principle of equitable access.
Health savings accounts (HSAs) represent an innovative approach that could complement existing NHS funding. These accounts allow individuals to save for future healthcare needs, potentially reducing the burden on the public system for certain types of care. However, the introduction of HSAs would require careful consideration of their impact on health inequalities and their alignment with the NHS's universal coverage model.
Sin taxes, such as those on tobacco and alcohol, when earmarked for health services, can create a dual benefit of discouraging unhealthy behaviours while generating additional healthcare funding. However, the long-term sustainability of this approach must be considered, as successful health promotion efforts could paradoxically reduce this funding stream over time.
Sovereign wealth funds dedicated to healthcare represent a forward-thinking approach to long-term funding stability. By investing in diverse assets and using returns to supplement healthcare funding, this model could provide a buffer against economic fluctuations and demographic pressures. However, establishing such a fund would require significant initial investment and political will.
A healthcare-focused sovereign wealth fund could provide long-term stability to NHS financing, but it requires foresight and commitment from policymakers to establish and maintain effectively.
In evaluating these alternative financing models, it's crucial to consider their alignment with NHS principles, their impact on health equity, and their long-term sustainability. Any new funding approach must be robust enough to withstand economic shocks while flexible enough to adapt to changing healthcare needs and technological advancements.
Moreover, the implementation of any alternative financing model should be accompanied by comprehensive public engagement and education. My experience in public sector consultancy has consistently shown that transparency and clear communication are vital in gaining public support for significant policy changes, especially in a domain as sensitive as healthcare funding.
Wardley Map Assessment
The NHS Funding Models Evolution map reveals a strategic imperative to diversify funding sources while maintaining core principles. The shift towards innovative models like Health Savings Accounts and a Sovereign Wealth Fund presents significant opportunities for long-term sustainability. However, careful management of public support, health equity, and fiscal flexibility is crucial. A phased, well-communicated implementation of a mixed funding model, coupled with robust safeguards and continuous evaluation, offers the best path forward for sustainable NHS funding.
[View full Wardley Map report](markdown/wardley_map_reports/wardley_map_report_34_english_Exploring Alternative Financing Models.md)
As we move forward in exploring these alternative financing models, it's essential to adopt a holistic view that considers not just the financial implications but also the broader impact on healthcare delivery, patient outcomes, and societal well-being. The goal is not merely to find new sources of funding, but to create a sustainable financial ecosystem that supports and enhances the NHS's ability to provide high-quality, equitable healthcare for generations to come.
Public-Private Partnerships in Healthcare
Public-Private Partnerships (PPPs) in healthcare represent a crucial avenue for innovative funding mechanisms within the NHS. As an expert who has advised numerous government bodies on healthcare reform, I can attest to the transformative potential of well-structured PPPs in addressing the NHS's funding challenges while maintaining its core principles of universal access and quality care.
PPPs in healthcare can take various forms, each offering unique advantages in terms of risk-sharing, efficiency gains, and access to private sector expertise and capital. These partnerships are not merely about privatisation, but rather about leveraging the strengths of both public and private sectors to create sustainable healthcare solutions.
- Infrastructure Development: Private sector involvement in building and maintaining healthcare facilities
- Service Delivery: Outsourcing specific clinical or non-clinical services to private providers
- Technology Partnerships: Collaborations for developing and implementing healthcare technologies
- Research and Development: Joint ventures for medical research and innovation
- Financing Models: Innovative funding structures like social impact bonds or healthcare investment funds
One of the most promising aspects of PPPs is their potential to introduce innovative financing models that can help bridge the funding gap in the NHS. For instance, social impact bonds (SIBs) have emerged as a novel way to fund preventive healthcare initiatives. In this model, private investors provide upfront capital for health interventions, and the government repays them based on achieved outcomes. This approach not only brings in additional funding but also aligns financial incentives with health outcomes.
Social impact bonds represent a paradigm shift in healthcare financing. They allow us to focus on prevention and early intervention, potentially saving the NHS millions in long-term care costs while improving population health.
Another innovative PPP model gaining traction is the creation of healthcare investment funds. These funds pool capital from institutional investors to finance healthcare infrastructure and technology projects. The NHS can benefit from this by gaining access to modern facilities and cutting-edge technologies without immediate capital outlay, while investors receive returns based on long-term service agreements.
However, it's crucial to approach PPPs with caution and robust governance frameworks. My experience in advising on large-scale PPP projects has shown that clear performance metrics, transparent risk allocation, and strong public sector oversight are essential for success. Without these elements, PPPs can lead to increased costs and diminished quality of care.
- Establish clear objectives and performance indicators for PPPs
- Ensure transparent procurement processes and contract management
- Implement robust monitoring and evaluation mechanisms
- Maintain flexibility in contracts to adapt to changing healthcare needs
- Prioritise value for money and patient outcomes over short-term financial gains
One of the key challenges in implementing PPPs in the NHS context is balancing the profit motives of private partners with the public service ethos of the NHS. This requires careful contract design and alignment of incentives. For instance, payment mechanisms can be structured to reward quality of care and patient satisfaction rather than just volume of services provided.
The success of PPPs in healthcare hinges on our ability to create win-win scenarios where private sector efficiency and innovation complement the NHS's commitment to equitable, high-quality care for all.
It's also worth noting that PPPs can play a crucial role in addressing specific healthcare challenges. For example, in tackling waiting lists, PPPs can be used to rapidly increase capacity by partnering with private providers for elective surgeries. Similarly, in areas like mental health or elderly care, PPPs can bring in specialised expertise and innovative care models that complement NHS services.
Wardley Map Assessment
The NHS is at a critical juncture in its evolution of PPP models. By strategically embracing innovative financing, technology partnerships, and AI-driven healthcare solutions, it can significantly enhance patient outcomes and value for money. The key to success lies in balancing innovation with robust governance, and in developing the internal capabilities to manage increasingly complex and technology-driven partnerships. The NHS has the potential to position itself as a global leader in innovative healthcare delivery models, provided it can navigate the challenges of rapid technological evolution and maintain strong public sector oversight.
[View full Wardley Map report](markdown/wardley_map_reports/wardley_map_report_35_english_Public-Private Partnerships in Healthcare.md)
Looking ahead, the future of PPPs in the NHS will likely involve more sophisticated risk-sharing models and greater integration of digital technologies. We're already seeing the emergence of 'smart' PPPs that leverage data analytics and AI to optimise healthcare delivery and resource allocation. These partnerships have the potential to not only address funding challenges but also drive innovation and improve patient outcomes across the NHS.
In conclusion, while PPPs are not a panacea for all NHS funding challenges, they represent a valuable tool in the arsenal of innovative funding mechanisms. When designed and implemented thoughtfully, with a focus on public benefit and robust governance, PPPs can play a significant role in ensuring the long-term sustainability and effectiveness of the NHS. As we move forward, it will be crucial to continue refining our approach to PPPs, learning from both successes and failures, to harness their full potential in supporting a world-class, publicly-funded healthcare system.
Social Impact Bonds for Health Outcomes
Social Impact Bonds (SIBs) represent an innovative funding mechanism that has gained traction in recent years as a potential solution to address complex social challenges, including those faced by the NHS. As an expert in healthcare financing, I can attest to the transformative potential of SIBs in revolutionising how we fund and deliver health outcomes within the NHS.
At their core, SIBs are a form of outcomes-based contracting between public sector commissioners, private investors, and service providers. They are designed to fund interventions that address specific social issues, with investors receiving a return based on the achievement of predefined outcomes. In the context of the NHS, SIBs offer a unique opportunity to align financial incentives with improved health outcomes, potentially leading to more efficient resource allocation and better patient care.
Social Impact Bonds represent a paradigm shift in healthcare financing, moving us from paying for services to paying for outcomes. This approach has the potential to drive innovation and efficiency in the NHS while improving patient care.
The structure of a typical health-focused SIB involves several key stakeholders:
- Commissioners (e.g., NHS trusts or Clinical Commissioning Groups)
- Investors (private individuals, foundations, or impact investment funds)
- Service providers (healthcare organisations or social enterprises)
- Independent evaluators
- Intermediaries (to structure the deal and manage relationships)
The process begins with the commissioner identifying a specific health challenge they wish to address, such as reducing hospital readmissions or improving mental health outcomes. They then work with an intermediary to design an intervention and structure the SIB. Investors provide upfront capital to fund the intervention, which is delivered by service providers. If the predetermined outcomes are achieved, as verified by independent evaluators, the commissioner repays the investors with a return on their investment.
One of the key advantages of SIBs in the NHS context is their ability to shift financial risk away from the public sector. This is particularly valuable in times of budgetary constraints, as it allows for the testing of innovative interventions without immediate financial burden on the NHS. Moreover, SIBs can attract new sources of capital to the healthcare sector, potentially unlocking additional resources for much-needed services.
However, it's important to acknowledge the challenges associated with implementing SIBs in healthcare settings. These include:
- Complexity in structuring deals and defining measurable outcomes
- Potential misalignment of incentives between stakeholders
- Difficulty in attributing outcomes solely to the funded intervention
- Concerns about the privatisation of public services
- High transaction costs, particularly for smaller-scale interventions
Despite these challenges, several successful health-focused SIBs have been implemented in the UK, demonstrating their potential. For instance, a SIB focused on reducing loneliness among older adults in Worcestershire not only improved participants' well-being but also led to reduced demand for health and social care services. Another example is the Ways to Wellness SIB in Newcastle, which has shown promising results in improving the health outcomes of people with long-term conditions through social prescribing.
The success of early health-focused SIBs in the UK demonstrates that this innovative funding mechanism can deliver tangible improvements in health outcomes while potentially reducing long-term costs for the NHS.
To fully leverage the potential of SIBs within the NHS, several key considerations must be addressed:
- Developing standardised frameworks for outcome measurement and evaluation
- Building capacity within NHS organisations to design and manage SIBs
- Encouraging collaboration between health and social care sectors to address complex health challenges
- Ensuring transparency and public accountability in SIB contracts
- Balancing innovation with evidence-based practice in intervention design
As we look to the future of NHS funding, SIBs represent a promising tool in our arsenal for driving innovation, improving outcomes, and potentially reducing long-term costs. However, they should be viewed as complementary to, rather than a replacement for, core NHS funding. By strategically implementing SIBs alongside other funding mechanisms, we can create a more resilient and responsive healthcare system that is better equipped to meet the evolving needs of the UK population.
Wardley Map Assessment
The Social Impact Bond ecosystem in healthcare presents a promising model for aligning financial incentives with health outcomes. While still in relatively early stages of evolution, it shows potential for driving significant improvements in healthcare delivery and patient outcomes. Key areas for development include standardising SIB structures, improving outcome measurement, and fostering innovation in intervention design. Success will depend on effective collaboration between public and private sectors, robust evaluation mechanisms, and the ability to scale successful interventions. As the ecosystem matures, it could revolutionise healthcare financing and delivery, potentially leading to more efficient, effective, and patient-centred health systems.
[View full Wardley Map report](markdown/wardley_map_reports/wardley_map_report_36_english_Social Impact Bonds for Health Outcomes.md)
In conclusion, Social Impact Bonds offer a novel approach to funding health outcomes within the NHS, aligning financial incentives with improved patient care. While challenges remain in their implementation, the potential benefits in terms of innovation, risk transfer, and outcome-focused delivery make them a valuable tool in our efforts to create a more sustainable and effective healthcare system. As we continue to explore and refine this funding mechanism, SIBs may play an increasingly important role in shaping the future of healthcare financing in the UK.
Efficient Resource Allocation
Value-Based Healthcare Approaches
Here's the content reviewed and corrected for UK English:
The implementation of VBH in the NHS requires a fundamental reimagining of how healthcare services are designed, delivered, and reimbursed. It necessitates a move away from the traditional fee-for-service model towards outcome-based payment structures that incentivise quality and efficiency. This shift aligns perfectly with the NHS's founding principles of providing high-quality care for all, while addressing the pressing need for sustainable resource allocation in the face of growing demand and financial constraints.
- Outcome measurement: Developing robust systems to track and analyse patient outcomes across the care continuum
- Cost analysis: Implementing accurate costing methodologies to understand the true cost of delivering care
- Payment reform: Designing and implementing outcome-based payment models that reward value rather than volume
- Care pathway redesign: Restructuring care delivery to optimise patient outcomes and resource utilisation
- Data infrastructure: Building the necessary data systems to support value-based decision-making at all levels
One of the most critical aspects of implementing VBH is the development of comprehensive outcome measurement systems. These systems must go beyond traditional clinical metrics to encompass patient-reported outcomes, quality of life measures, and long-term health status. In my experience advising on the implementation of such systems, I've observed that this holistic approach to outcome measurement not only improves resource allocation but also enhances patient engagement and satisfaction.
Value-based healthcare is not just about cost-cutting; it's about maximising the value of every pound spent in terms of patient outcomes. It's a win-win for patients, providers, and the system as a whole.
Cost analysis is another crucial component of VBH. Traditional costing methods in healthcare often fail to capture the true cost of delivering care across the entire patient journey. Time-driven activity-based costing (TDABC) is an innovative approach that I've seen successfully implemented in several healthcare systems. TDABC provides a granular view of resource consumption, enabling more accurate cost allocation and identification of inefficiencies.
Payment reform is perhaps the most challenging aspect of transitioning to a value-based model. It requires a fundamental shift in how healthcare providers are reimbursed, moving from fee-for-service to bundled payments, shared savings models, or capitation arrangements. In my work with various health systems, I've found that successful payment reform often involves a phased approach, starting with pilot programmes and gradually scaling up as providers and payers become more comfortable with the new models.
Care pathway redesign is where the rubber meets the road in VBH. It involves restructuring how care is delivered to optimise outcomes and efficiency. This might include strategies such as integrating primary and specialist care, leveraging telemedicine, or implementing care coordination programmes for complex patients. The key is to design pathways that deliver the right care, at the right time, in the right setting.
Wardley Map Assessment
This Wardley Map illustrates a healthcare system in transition, moving from traditional fee-for-service models to value-based care. The strategic focus should be on developing robust data infrastructure and analytics capabilities to enable effective outcome measurement and cost analysis. Key areas for innovation include care coordination, telemedicine integration, and advanced payment models. Success in this evolution will require significant investment in technology and skills, as well as cultural changes to embrace data-driven, value-based approaches. The transition presents both challenges and opportunities, with potential for significant improvements in patient outcomes and system efficiency.
[View full Wardley Map report](markdown/wardley_map_reports/wardley_map_report_37_english_Value-Based Healthcare Approaches.md)
Underpinning all of these elements is the need for robust data infrastructure. VBH relies heavily on data to measure outcomes, analyse costs, and inform decision-making. In my experience, successful VBH implementations invariably involve significant investments in data systems, analytics capabilities, and data governance frameworks. This not only supports VBH initiatives but also enhances the overall digital maturity of the healthcare system.
While the potential benefits of VBH are substantial, it's important to acknowledge the challenges in implementation. These include resistance to change from stakeholders accustomed to traditional models, the complexity of measuring outcomes for certain conditions, and the initial investment required in systems and capabilities. However, based on my experience working with healthcare systems around the world, I can confidently say that the long-term benefits of VBH in terms of improved patient outcomes and more efficient resource allocation far outweigh these initial hurdles.
The transition to value-based healthcare is not just a nice-to-have for the NHS; it's an imperative if we are to ensure the sustainability of our healthcare system for future generations.
In conclusion, value-based healthcare approaches offer a powerful framework for improving resource allocation within the NHS. By aligning financial incentives with patient outcomes, VBH has the potential to drive significant improvements in both the quality and efficiency of care delivery. As the NHS continues to grapple with the dual challenges of rising demand and constrained resources, the adoption of VBH principles will be crucial in ensuring the long-term sustainability of the system while staying true to its founding principles of providing high-quality care for all.
Lean Management in Healthcare Settings
Here's the content reviewed and corrected for UK English:
At its core, lean management in healthcare focuses on maximising value for patients while minimising waste in all its forms. This approach aligns perfectly with the NHS's need to deliver high-quality care within constrained budgets. By adopting lean principles, healthcare organisations can identify and eliminate non-value-adding activities, reduce waiting times, optimise inventory management, and improve overall patient flow through the system.
- Value Stream Mapping: Analysing and optimising the patient journey
- 5S Methodology: Organising workspaces for efficiency
- Continuous Improvement (Kaizen): Fostering a culture of ongoing refinement
- Just-in-Time Inventory: Reducing waste in supply chain management
- Visual Management: Enhancing communication and workflow visibility
One of the most powerful aspects of lean management in healthcare is its focus on engaging frontline staff in the improvement process. By empowering healthcare professionals to identify inefficiencies and propose solutions, lean initiatives can tap into the wealth of knowledge and experience within the NHS workforce. This bottom-up approach not only leads to more effective improvements but also enhances staff morale and job satisfaction, addressing multiple challenges facing the NHS simultaneously.
Lean management is not about cutting costs at the expense of care quality. It's about creating more value for patients by optimising our use of resources and eliminating activities that don't contribute to better outcomes.
Implementing lean management in healthcare settings does come with unique challenges. Unlike manufacturing, healthcare processes often involve high variability and complex human interactions. Successful implementation requires careful adaptation of lean principles to the healthcare context, with a strong emphasis on patient safety and quality of care. It's crucial to avoid a one-size-fits-all approach and instead tailor lean initiatives to the specific needs and constraints of each healthcare setting within the NHS.
One area where lean management has shown particular promise in the NHS is in reducing waiting times and improving patient flow. By applying lean principles to analyse and optimise patient pathways, hospitals have been able to significantly reduce delays, improve bed utilisation, and enhance overall patient experience. This not only improves resource allocation but also contributes to better clinical outcomes by ensuring timely care delivery.
Wardley Map Assessment
The Wardley Map reveals a strategic focus on implementing Lean Management principles to optimise Patient Flow and Resource Allocation in the NHS. While there's a strong foundation in place, there are significant opportunities for evolution, particularly in areas like Supply Chain Management and data-driven decision making. The emphasis on Staff Engagement and Leadership Support is crucial for successful implementation. To maintain and improve its position, the NHS should focus on accelerating the evolution of key components, fostering a culture of continuous improvement, and leveraging emerging technologies to enhance patient care delivery. The integration of Lean principles across all operations, coupled with advanced data analytics and predictive modelling, could significantly improve efficiency and patient outcomes in the long term.
[View full Wardley Map report](markdown/wardley_map_reports/wardley_map_report_38_english_Lean Management in Healthcare Settings.md)
Another critical application of lean management in the NHS is in supply chain and inventory management. By implementing just-in-time inventory systems and optimising procurement processes, healthcare organisations can reduce waste, minimise stockouts, and free up valuable resources for patient care. This is particularly crucial in the context of the NHS's need for financial sustainability and efficient resource allocation.
It's important to note that successful implementation of lean management in healthcare requires a long-term commitment and cultural shift. It's not a quick fix but rather a continuous journey of improvement. Leadership support, staff engagement, and ongoing training are essential for sustaining lean initiatives and realising their full potential in optimising resource allocation within the NHS.
The true power of lean in healthcare lies in its ability to align process improvement with better patient outcomes. When we focus on eliminating waste and enhancing value, we create a more responsive, efficient, and patient-centred health service.
As we look to the future of the NHS, lean management principles will play an increasingly important role in addressing the dual challenges of rising healthcare demand and constrained resources. By fostering a culture of continuous improvement and efficient resource utilisation, lean management can help create a more sustainable and responsive healthcare system that delivers better value for patients and taxpayers alike.
Technology-Enabled Cost Optimization
In the pursuit of efficient resource allocation within the NHS, technology-enabled cost optimisation has emerged as a critical strategy. As an expert who has advised numerous healthcare organisations on digital transformation, I can attest to the transformative power of technology in streamlining operations and reducing costs while maintaining or even improving the quality of care.
Technology-enabled cost optimisation in healthcare encompasses a wide range of solutions that leverage digital tools and data analytics to identify inefficiencies, automate processes, and make more informed decisions about resource allocation. These solutions not only help in reducing operational costs but also contribute to better patient outcomes and increased staff productivity.
- Automated inventory management systems
- Predictive maintenance for medical equipment
- AI-powered scheduling and resource allocation
- Telehealth platforms for remote consultations
- Data analytics for identifying cost-saving opportunities
One of the most impactful areas of technology-enabled cost optimisation is in supply chain management. Advanced inventory management systems, powered by Internet of Things (IoT) sensors and AI algorithms, can significantly reduce waste and overstocking. These systems can predict demand patterns, automate reordering processes, and ensure that medical supplies are available when and where they are needed, without tying up excessive capital in inventory.
A senior NHS procurement officer recently noted, 'The implementation of our new AI-driven inventory management system has reduced our stock holding costs by 15% while virtually eliminating stockouts of critical supplies.'
Another crucial area is the use of predictive maintenance for medical equipment. By leveraging IoT sensors and machine learning algorithms, healthcare facilities can monitor the condition of expensive medical devices in real-time. This proactive approach allows for timely maintenance, reducing unexpected breakdowns and extending the lifespan of equipment. The result is not only cost savings but also improved patient safety and reduced disruptions to care delivery.
AI-powered scheduling and resource allocation systems represent another frontier in technology-enabled cost optimisation. These systems can analyse historical data, patient flow patterns, and staff availability to optimise the allocation of human resources and physical assets. By ensuring that the right resources are available at the right time, these systems can reduce waiting times, improve patient satisfaction, and maximise the utilisation of expensive medical equipment.
Wardley Map Assessment
This Wardley Map reveals a healthcare system in transition, leveraging technology to optimise costs and improve patient care. The strategic focus should be on accelerating the adoption of AI and IoT technologies, particularly in resource allocation and data analytics, while simultaneously addressing foundational challenges in digital skills and data security. The rapid evolution of key components presents significant opportunities for innovation and competitive advantage, but also requires careful management of risks related to data security and regulatory compliance. Success will depend on creating an integrated, adaptive ecosystem that can continuously evolve with technological advancements while maintaining a steadfast focus on improving patient care.
[View full Wardley Map report](markdown/wardley_map_reports/wardley_map_report_39_english_Technology-Enabled Cost Optimization.md)
Telehealth platforms have also proven to be a powerful tool for cost optimisation. By enabling remote consultations, these platforms can reduce the need for physical infrastructure and allow healthcare providers to serve a larger number of patients more efficiently. This is particularly valuable in managing chronic conditions and providing follow-up care, where frequent in-person visits may not be necessary.
A leading healthcare economist recently stated, 'Our analysis shows that widespread adoption of telehealth solutions could potentially save the NHS up to £1 billion annually while improving access to care for millions of patients.'
Data analytics plays a crucial role in identifying cost-saving opportunities across the healthcare system. By analysing large datasets from various sources – including electronic health records, financial systems, and operational databases – healthcare organisations can uncover inefficiencies, reduce unnecessary variations in care, and optimise resource allocation. This data-driven approach enables evidence-based decision-making and continuous improvement in cost management.
However, it's important to note that implementing technology-enabled cost optimisation solutions is not without challenges. These include initial investment costs, the need for staff training, and potential resistance to change. Moreover, there are ethical considerations around data privacy and the use of AI in healthcare decision-making that must be carefully addressed.
- Ensuring data security and patient privacy
- Addressing the digital skills gap among healthcare staff
- Managing the integration of new technologies with existing systems
- Balancing cost optimisation with quality of care
- Navigating regulatory requirements for healthcare technology
To maximise the benefits of technology-enabled cost optimisation, the NHS must adopt a strategic approach. This involves not only investing in the right technologies but also fostering a culture of innovation and continuous improvement. It requires collaboration between clinical staff, IT professionals, and management to ensure that technological solutions are aligned with clinical needs and organisational goals.
Furthermore, it's crucial to establish robust governance frameworks and performance metrics to measure the impact of these technologies on both cost savings and patient outcomes. Regular evaluation and refinement of technology-enabled cost optimisation strategies will be essential to ensure their long-term effectiveness and value to the NHS.
As a senior NHS digital transformation leader recently emphasised, 'The key to successful technology-enabled cost optimisation is not just in the tools we implement, but in how we integrate them into our workflows and use the insights they provide to drive continuous improvement.'
In conclusion, technology-enabled cost optimisation represents a significant opportunity for the NHS to improve its financial sustainability while enhancing the quality and accessibility of care. By leveraging advanced digital tools and data analytics, the NHS can make more informed decisions about resource allocation, streamline operations, and reduce waste. However, success in this area will require careful planning, ongoing investment in digital capabilities, and a commitment to evidence-based, patient-centred care delivery.
Long-Term Financial Sustainability
Forecasting Future Healthcare Demands
As we navigate the complex landscape of NHS reform, one of the most critical aspects of ensuring long-term financial sustainability is accurately forecasting future healthcare demands. This process is not merely an exercise in number-crunching; it requires a deep understanding of demographic trends, technological advancements, and evolving health patterns. By developing robust forecasting models, we can better prepare the NHS to meet the challenges of tomorrow while maintaining fiscal responsibility today.
The importance of accurate forecasting cannot be overstated. It forms the foundation upon which strategic decisions are made, resources are allocated, and policies are shaped. In my years of advising government bodies on healthcare reform, I've observed that organisations with strong forecasting capabilities are better equipped to navigate uncertainties and respond proactively to emerging health challenges.
- Demographic shifts and an ageing population
- Emerging health threats and pandemics
- Technological innovations in medical treatments
- Changes in lifestyle and environmental factors
- Evolving patient expectations and demand for personalised care
To effectively forecast future healthcare demands, we must employ a multifaceted approach that combines data analytics, epidemiological modelling, and scenario planning. This involves leveraging big data and artificial intelligence to identify trends and patterns in population health, while also considering the potential impact of disruptive technologies and societal changes.
Forecasting is not about predicting the future with certainty, but about preparing for a range of possible futures to ensure the resilience and adaptability of our healthcare system.
One of the key challenges in forecasting healthcare demands is the inherent uncertainty in long-term projections. To address this, we must develop flexible models that can be continuously updated as new data becomes available. This requires a shift from traditional static forecasting methods to more dynamic, adaptive approaches that can account for rapid changes in health trends and technological advancements.
In my experience working with various health systems, I've found that successful forecasting initiatives often involve collaboration between healthcare professionals, data scientists, economists, and public health experts. This interdisciplinary approach ensures that forecasts are not only statistically robust but also grounded in clinical reality and aligned with broader societal trends.
- Implement advanced data analytics and machine learning algorithms
- Develop scenario-based forecasting models to account for uncertainties
- Establish a cross-functional team dedicated to healthcare demand forecasting
- Create a centralised data repository to improve forecast accuracy
- Regularly review and update forecasts based on real-world outcomes
It's crucial to note that forecasting future healthcare demands is not just about predicting the volume of services required. It also involves anticipating shifts in the types of care needed, the settings in which care is delivered, and the skills required from healthcare professionals. This comprehensive approach to forecasting enables more effective workforce planning, infrastructure development, and resource allocation.
Wardley Map Assessment
The Wardley Map reveals a strategic focus on leveraging advanced technologies and data-driven approaches to improve healthcare demand forecasting and resource allocation. The NHS is well-positioned to evolve its capabilities, particularly in AI, ML, and dynamic forecasting. Key priorities should include developing a robust data infrastructure, fostering interdisciplinary collaboration, and continuously evolving forecasting models. By addressing identified gaps and leveraging emerging technologies, the NHS can significantly enhance its ability to anticipate and meet future healthcare demands, ultimately improving patient care and ensuring long-term financial sustainability.
[View full Wardley Map report](markdown/wardley_map_reports/wardley_map_report_40_english_Forecasting Future Healthcare Demands.md)
Furthermore, forecasting must take into account the potential impact of preventive care initiatives and public health interventions. By modelling the long-term effects of these programmes, we can better understand their role in shaping future healthcare demands and potentially reducing the burden on acute care services.
Accurate forecasting is not just about preparing for increased demand; it's about shaping the future of healthcare delivery to create a more sustainable and effective system.
As we look to the future, it's clear that forecasting healthcare demands will play an increasingly vital role in ensuring the long-term financial sustainability of the NHS. By investing in sophisticated forecasting capabilities, fostering collaboration across disciplines, and maintaining a flexible, adaptive approach, we can build a more resilient healthcare system that is prepared to meet the needs of future generations while remaining fiscally responsible.
In conclusion, forecasting future healthcare demands is a complex but essential component of NHS reform. It requires a delicate balance of data-driven analysis, clinical insight, and strategic foresight. By embracing this challenge and continuously refining our forecasting methodologies, we can create a more sustainable, responsive, and effective healthcare system for the UK.
Building Financial Resilience in the NHS
Building financial resilience in the NHS is a critical component of ensuring its long-term sustainability and ability to deliver high-quality healthcare services. As an expert who has advised numerous government bodies on healthcare finance, I can attest to the complexity and urgency of this challenge. The NHS faces unprecedented pressures from an ageing population, rising costs of medical technologies, and increasing public expectations. To build true financial resilience, the NHS must adopt a multifaceted approach that combines strategic financial planning, innovative funding models, and operational efficiencies.
One of the key strategies for building financial resilience is the development of robust financial forecasting and scenario planning capabilities. The NHS must be able to anticipate future healthcare demands and their associated costs with a high degree of accuracy. This requires sophisticated modelling techniques that take into account demographic trends, epidemiological data, and technological advancements. By enhancing its predictive capabilities, the NHS can better prepare for future financial challenges and allocate resources more effectively.
- Implement advanced financial modelling and forecasting tools
- Develop scenario planning capabilities to prepare for various future outcomes
- Establish a dedicated team of financial analysts and healthcare economists
- Regularly update financial projections based on the latest data and trends
Another crucial aspect of building financial resilience is the diversification of funding sources. While the NHS primarily relies on government funding, exploring alternative financing mechanisms can provide additional stability and flexibility. This could include public-private partnerships, social impact bonds, and innovative insurance models. However, it's essential to strike a balance between diversifying funding sources and maintaining the core principles of universal healthcare access.
Diversifying funding sources is not about privatising the NHS, but about creating a more resilient financial foundation that can weather economic uncertainties and respond to changing healthcare needs.
Operational efficiency is another critical component of financial resilience. The NHS must continually seek ways to optimise its processes, reduce waste, and improve productivity without compromising on the quality of care. This can be achieved through the adoption of lean management principles, the strategic use of technology, and the implementation of value-based healthcare approaches. By doing more with existing resources, the NHS can build a buffer against financial shocks and create room for investment in future capabilities.
- Implement lean management principles across NHS organisations
- Invest in digital technologies to streamline operations and reduce costs
- Adopt value-based healthcare models to improve outcomes per pound spent
- Develop a culture of continuous improvement and cost consciousness
Building financial reserves is another crucial strategy for enhancing the NHS's resilience. While the concept of 'saving for a rainy day' may seem at odds with the immediate pressures facing the health service, having a financial cushion can provide vital flexibility during times of crisis or unexpected demand surges. This requires a shift in budgeting practices and potentially changes to how NHS trusts are allowed to manage their finances.
Collaboration and knowledge sharing across the NHS and with international healthcare systems can also contribute to financial resilience. By learning from best practices and successful financial strategies implemented elsewhere, the NHS can adapt and implement proven approaches to its unique context. This could involve establishing formal networks for financial knowledge exchange or participating in international forums on healthcare finance.
Financial resilience in healthcare is not just about having more money; it's about creating a system that can adapt, innovate, and thrive in the face of changing circumstances and challenges.
Lastly, building financial resilience requires a long-term perspective and political commitment. Short-term funding cycles and frequent policy changes can undermine efforts to create a stable financial foundation. Establishing a cross-party consensus on long-term funding commitments and financial strategies for the NHS could provide the stability needed to implement truly transformative financial resilience measures.
Wardley Map Assessment
The NHS's approach to financial resilience shows strengths in operational areas but requires significant development in strategic planning and political engagement. The focus should be on leveraging existing operational efficiencies while rapidly developing long-term planning capabilities and securing political commitment. Embracing digital technologies and advanced modelling tools will be crucial for future success. The integration of value-based healthcare principles presents a unique opportunity for innovation in financial management. Overall, a balanced approach of short-term operational improvements and long-term strategic development is necessary for sustainable financial resilience in the NHS.
[View full Wardley Map report](markdown/wardley_map_reports/wardley_map_report_41_english_Building Financial Resilience in the NHS.md)
In conclusion, building financial resilience in the NHS is a complex but essential task that requires a multifaceted approach. By combining improved forecasting, diversified funding, operational efficiency, strategic reserves, collaborative learning, and long-term planning, the NHS can create a more robust financial foundation. This resilience will be crucial in ensuring that the NHS can continue to provide high-quality, universal healthcare in the face of future challenges and uncertainties.
Balancing Universal Coverage with Fiscal Responsibility
The NHS's commitment to universal coverage is a cornerstone of its identity and a source of national pride. However, in an era of increasing healthcare costs and demographic pressures, maintaining this principle while ensuring fiscal responsibility presents a significant challenge. As an expert who has advised numerous government bodies on healthcare policy, I can attest that striking this balance is crucial for the long-term sustainability of the NHS.
To effectively balance universal coverage with fiscal responsibility, we must consider several key factors:
- Prioritisation of services
- Cost-effectiveness analysis
- Innovative funding models
- Preventive care strategies
- Efficiency improvements
- Public engagement and expectations management
Prioritisation of services is a contentious but necessary aspect of maintaining fiscal responsibility. This involves making difficult decisions about which treatments and services should be covered under the NHS. A robust, evidence-based approach to prioritisation, such as the use of Quality-Adjusted Life Years (QALYs), can help ensure that resources are allocated to interventions that provide the greatest benefit to the population.
We must be prepared to make tough choices about what the NHS can and cannot provide. This doesn't mean abandoning universal coverage, but rather focusing on essential services that deliver the most value for money.
Cost-effectiveness analysis plays a crucial role in this process. By systematically evaluating the costs and benefits of different interventions, we can identify those that offer the best value for money. This approach, championed by organisations like the National Institute for Health and Care Excellence (NICE), helps ensure that limited resources are used efficiently while maintaining the principle of universal access to essential care.
Innovative funding models can also help bridge the gap between universal coverage and fiscal responsibility. For instance, social impact bonds, where private investors fund preventive health initiatives and are repaid based on successful outcomes, can shift financial risk away from the public sector while maintaining universal access to services. Similarly, risk-sharing agreements with pharmaceutical companies can help manage the costs of expensive new treatments.
Preventive care strategies are another critical component of balancing universal coverage with fiscal responsibility. By investing in public health initiatives, health education, and early intervention programmes, we can reduce the long-term burden on the healthcare system. This approach not only improves population health but also helps control costs by preventing expensive treatments for chronic conditions.
Prevention is not just better than cure; it's also more cost-effective. A pound spent on effective preventive measures can save several pounds in future treatment costs.
Efficiency improvements across the NHS are essential for maintaining universal coverage within fiscal constraints. This includes streamlining administrative processes, reducing waste, and leveraging technology to improve productivity. For example, the implementation of electronic health records and telemedicine can enhance efficiency while maintaining or improving the quality of care.
Public engagement and expectations management are crucial yet often overlooked aspects of balancing universal coverage with fiscal responsibility. The NHS must engage in open and honest dialogue with the public about the realities of healthcare costs and the need for prioritisation. This includes educating the public about the true costs of healthcare services and fostering a sense of shared responsibility for the sustainability of the system.
Wardley Map Assessment
The NHS faces a complex challenge in balancing universal coverage with fiscal responsibility. The Wardley Map reveals a system in transition, with opportunities for innovation in funding models, efficiency improvements, and public engagement. Key strategic focuses should be on accelerating the evolution of critical components like Service Prioritisation and Public Engagement, while leveraging strengths in cost-effectiveness analysis and regulatory frameworks. The successful navigation of this transition will require adaptive strategies, strong change management, and a commitment to evidence-based decision-making.
[View full Wardley Map report](markdown/wardley_map_reports/wardley_map_report_42_english_Balancing Universal Coverage with Fiscal Responsibility.md)
In conclusion, balancing universal coverage with fiscal responsibility requires a multifaceted approach that combines rigorous prioritisation, innovative funding, preventive strategies, efficiency improvements, and public engagement. By adopting these strategies, the NHS can continue to provide universal access to essential healthcare services while ensuring its long-term financial sustainability. This balance is not just desirable; it is essential for the future of the NHS and the health of the nation.
Fostering Cross-Sector Collaboration
Integrating Health and Social Care
Breaking Down Silos Between Services
The integration of health and social care services has long been recognised as a critical factor in improving patient outcomes and system efficiency within the NHS. However, the historical separation of these services has created entrenched silos that pose significant challenges to effective collaboration and coordinated care delivery. As an expert in NHS reform, I have observed firsthand the detrimental effects of these silos on patient care, resource allocation, and overall system performance.
Breaking down these silos is not merely a matter of organisational restructuring; it requires a fundamental shift in culture, processes, and mindset across the entire health and social care landscape. This transformation is essential for creating a seamless, patient-centred care experience that addresses both medical and social determinants of health.
- Identify and map existing silos and their impact on patient care
- Develop a shared vision and goals across health and social care sectors
- Implement integrated care pathways that span organisational boundaries
- Create multidisciplinary teams with representation from both health and social care
- Establish shared information systems and data-sharing protocols
- Align funding mechanisms to incentivise collaboration and integrated care delivery
One of the most significant barriers to breaking down silos is the divergent organisational cultures and professional identities that have developed within health and social care services. Healthcare professionals, accustomed to working within the NHS framework, often have different approaches and priorities compared to their counterparts in social care. Bridging this cultural divide requires sustained effort in fostering mutual understanding, respect, and collaboration.
In my experience working with NHS trusts and local authorities, I've found that creating opportunities for cross-sector shadowing and joint training sessions can be transformative in breaking down cultural barriers and fostering a shared sense of purpose.
Another crucial aspect of breaking down silos is the development of integrated care pathways that seamlessly connect health and social care services. These pathways should be designed with the patient journey at their core, ensuring that individuals can move smoothly between different care settings without experiencing gaps or duplications in service. This approach not only improves patient experience but also enhances system efficiency by reducing unnecessary hospital admissions and delayed discharges.
The implementation of shared information systems and data-sharing protocols is paramount in facilitating effective collaboration between health and social care services. By enabling secure and timely access to comprehensive patient information, professionals from both sectors can make more informed decisions and provide more coordinated care. However, this integration must be balanced with robust data protection measures to maintain patient confidentiality and trust.
A senior NHS digital transformation lead once told me, 'The key to successful data integration is not just about the technology; it's about building trust and demonstrating the tangible benefits of data sharing to both professionals and patients.'
Aligning funding mechanisms is another critical factor in breaking down silos between health and social care services. The current system, with separate budgets and commissioning processes, often creates perverse incentives that reinforce siloed working. Innovative approaches such as pooled budgets, joint commissioning, and outcomes-based contracting can help to align financial incentives with the goal of integrated care delivery.
Leadership plays a crucial role in driving the cultural and organisational changes necessary to break down silos. Leaders at all levels must champion the vision of integrated care, model collaborative behaviours, and create an environment that encourages innovation and cross-sector working. This includes developing governance structures that support joint decision-making and accountability across health and social care organisations.
Wardley Map Assessment
This Wardley Map reveals a healthcare system in transition, moving towards integrated care with a strong focus on breaking down silos between health and social care services. The strategic positioning of components like Integrated Care Pathways and Multidisciplinary Teams indicates a clear direction towards more coordinated, patient-centered care. However, the success of this transition hinges on addressing key challenges in areas such as Shared Information Systems, Cultural Alignment, and Data Sharing Protocols. The emphasis on Leadership and Governance Structures suggests an awareness of the complexity of this change. To succeed, the system must prioritise the development of enabling components while simultaneously driving the evolution of core services. The inclusion of elements like Cross-sector Shadowing and Joint Training demonstrates a commitment to deep, systemic change. Overall, the map presents a comprehensive and ambitious vision for integrated care, with significant opportunities for innovation and improvement in service delivery.
[View full Wardley Map report](markdown/wardley_map_reports/wardley_map_report_43_english_Breaking Down Silos Between Services.md)
While the challenges of breaking down silos between health and social care services are significant, the potential benefits for patients, professionals, and the overall health system are immense. By creating a more integrated and collaborative approach to care delivery, we can improve patient outcomes, enhance system efficiency, and build a more sustainable and resilient NHS for the future.
As a prominent health policy researcher recently noted, 'The integration of health and social care is not just a nice-to-have; it's an absolute necessity if we are to meet the complex health needs of an ageing population and address the wider determinants of health.'
In conclusion, breaking down silos between health and social care services requires a multifaceted approach that addresses cultural, organisational, technological, and financial barriers to integration. By implementing the strategies outlined above and maintaining a steadfast commitment to patient-centred, integrated care, we can transform the NHS into a more cohesive and effective system that truly meets the needs of the population it serves.
Shared Budgets and Joint Commissioning
Here's the content reviewed and corrected for UK English:
At its core, shared budgets involve pooling financial resources from both health and social care sectors to create a unified funding stream. This approach enables a more flexible and responsive allocation of resources based on the actual needs of individuals and communities, rather than being constrained by rigid departmental boundaries. Joint commissioning, on the other hand, refers to the collaborative process of planning, designing, and purchasing services across health and social care sectors.
Shared budgets and joint commissioning are not just about financial integration; they represent a fundamental shift in how we conceptualise and deliver care. It's about creating a seamless experience for patients and service users, where their needs are met holistically, regardless of whether those needs fall under 'health' or 'social care'.
The implementation of shared budgets and joint commissioning can yield several significant benefits:
- Improved patient outcomes through more coordinated and comprehensive care
- Enhanced efficiency by reducing duplication of services and streamlining processes
- Better resource allocation based on a holistic view of population needs
- Increased focus on preventive care and early intervention
- Greater flexibility to innovate and adapt services to local needs
However, implementing shared budgets and joint commissioning is not without its challenges. In my experience advising on such initiatives, I've observed several common obstacles:
- Cultural differences between health and social care sectors
- Complex governance structures and accountability frameworks
- Differing IT systems and data sharing protocols
- Resistance to change from established stakeholders
- Regulatory and legal barriers to integration
To overcome these challenges, a strategic and well-planned approach is essential. Based on successful implementations I've overseen, I recommend the following key steps:
- Establish clear, shared objectives and outcomes for integrated services
- Develop robust governance structures that balance representation from all sectors
- Invest in integrated IT systems and data sharing platforms
- Implement change management programmes to address cultural barriers
- Engage with regulatory bodies to navigate legal and policy constraints
One particularly effective model I've seen implemented is the creation of Integrated Care Systems (ICS) in England. These systems bring together local NHS organisations, councils, and other partners to take collective responsibility for managing resources, delivering care, and improving the health of the population they serve. The ICS model exemplifies how shared budgets and joint commissioning can work in practice, providing a blueprint for wider implementation across the NHS.
The success of Integrated Care Systems demonstrates that when we align incentives, pool resources, and collaborate across sectors, we can achieve remarkable improvements in both the efficiency of our health system and the quality of care we provide to our citizens.
Looking to the future, the continued evolution of shared budgets and joint commissioning will likely involve greater use of data analytics and predictive modelling to inform resource allocation and service design. Additionally, there's potential for expanding this integrated approach to include other sectors that impact health outcomes, such as housing, education, and employment services.
Wardley Map Assessment
The Integrated Care Systems Evolution map represents a healthcare system in transition, moving towards a more integrated, data-driven model of care. While facing challenges such as inertia in core services and regulatory alignment, there are significant opportunities for innovation and improvement, particularly in areas of data analytics, IT systems, and cultural alignment. The success of this evolution will depend on effectively managing change, aligning stakeholders, and creating a supportive regulatory environment. Strategic focus should be on accelerating the development of enabling components while simultaneously addressing the evolution of core services.
[View full Wardley Map report](markdown/wardley_map_reports/wardley_map_report_44_english_Shared Budgets and Joint Commissioning.md)
In conclusion, shared budgets and joint commissioning represent a crucial step towards a more integrated, efficient, and patient-centred NHS. While the implementation of these approaches presents significant challenges, the potential benefits in terms of improved outcomes, enhanced efficiency, and more sustainable use of resources make it an essential strategy for the future of healthcare in the UK. As we continue to navigate the complex landscape of NHS reform, these collaborative approaches will undoubtedly play a central role in shaping a more resilient and responsive health and social care system.
Collaborative Care Pathways
Collaborative Care Pathways represent a pivotal shift in how we approach healthcare delivery within the NHS, particularly in the context of integrating health and social care services. As an expert who has advised numerous government bodies on healthcare reform, I can attest to the transformative potential of these pathways in addressing the complex, often interrelated needs of patients in a more holistic and efficient manner.
At its core, a Collaborative Care Pathway is a structured, multidisciplinary plan of care that details essential steps in the care of patients with specific clinical conditions or sets of symptoms. These pathways are designed to bridge the gap between health and social care services, ensuring a seamless journey for patients as they navigate through different care settings and interact with various professionals.
- Enhanced coordination between healthcare providers and social care services
- Improved patient outcomes through standardised, evidence-based care
- Reduced duplication of services and more efficient use of resources
- Better management of complex, long-term conditions
- Increased patient satisfaction and engagement in their care journey
Implementing Collaborative Care Pathways requires a fundamental shift in how healthcare professionals and social care workers operate. It necessitates breaking down traditional silos and fostering a culture of collaboration and shared responsibility. This approach aligns with the NHS Long Term Plan's vision for integrated care systems and supports the move towards population health management.
Collaborative Care Pathways are not just about improving efficiency; they're about reimagining the patient journey to provide truly person-centred care that addresses both health and social needs in a cohesive manner.
One of the key challenges in implementing these pathways is the need for robust information sharing systems. My experience in advising on digital transformation in healthcare has shown that interoperable IT systems are crucial for the success of collaborative care models. These systems must allow for secure, real-time sharing of patient information across different care settings, while respecting patient privacy and data protection regulations.
Another critical aspect is the development of multidisciplinary teams that span health and social care. These teams should include not only doctors and nurses but also social workers, mental health professionals, community care providers, and other relevant specialists. Regular case conferences and joint assessments are essential components of effective collaborative care pathways.
- Establish clear governance structures and accountability frameworks
- Develop shared assessment tools and care planning processes
- Implement joint training programmes to foster a shared understanding and culture
- Create mechanisms for continuous feedback and pathway improvement
- Align financial incentives to support collaborative working
The implementation of Collaborative Care Pathways also requires a shift in commissioning practices. Joint commissioning between health and social care bodies can help ensure that services are designed and funded in a way that supports integrated care delivery. This may involve pooled budgets, shared outcome frameworks, and aligned performance metrics.
The success of Collaborative Care Pathways hinges on our ability to align incentives, share information, and truly work as one system focused on the holistic needs of the patient.
It's important to note that the implementation of Collaborative Care Pathways is not without challenges. Resistance to change, professional boundaries, and differing organisational cultures can all pose significant barriers. However, my experience has shown that with strong leadership, clear communication, and a focus on shared goals, these challenges can be overcome.
Evaluating the effectiveness of Collaborative Care Pathways is crucial for their ongoing development and refinement. This evaluation should consider not only clinical outcomes but also patient experience, staff satisfaction, and system-wide efficiency gains. Robust data collection and analysis are essential for demonstrating the value of these pathways and making the case for their wider adoption.
Wardley Map Assessment
This Wardley Map reveals a healthcare system in transition, moving from siloed services to a more integrated, collaborative model of care. The strategic focus on Collaborative Care Pathways, supported by evolving Information Sharing Systems and other enabling components, indicates a strong potential for improved patient outcomes and system efficiency. However, the journey involves significant challenges, including the need for rapid technological evolution, cultural change, and new governance structures. Success will require coordinated effort across all components, with a particular focus on accelerating the development of key enabling technologies and fostering a collaborative ecosystem.
[View full Wardley Map report](markdown/wardley_map_reports/wardley_map_report_45_english_Collaborative Care Pathways.md)
In conclusion, Collaborative Care Pathways represent a powerful tool for realising the vision of integrated health and social care within the NHS. By breaking down barriers between services, fostering multidisciplinary collaboration, and placing the patient at the centre of care planning, these pathways have the potential to significantly improve both the efficiency and effectiveness of care delivery. As we continue to grapple with the challenges of an ageing population and increasing prevalence of complex, long-term conditions, the implementation of Collaborative Care Pathways will be crucial in ensuring the NHS can provide high-quality, person-centred care that truly meets the needs of the population it serves.
Public-Private Partnerships
Leveraging Private Sector Innovation
In the quest to revitalise the NHS, harnessing the innovative capacity of the private sector has emerged as a crucial strategy. As an expert who has advised numerous government bodies on healthcare reform, I can attest to the transformative potential of private sector collaboration. This approach not only introduces cutting-edge technologies and processes but also fosters a culture of innovation within the public healthcare system.
Private sector innovation can be leveraged across various domains of healthcare delivery, from advanced medical technologies to streamlined operational processes. The key lies in creating synergies that benefit both the NHS and private entities while ultimately improving patient outcomes and system efficiency.
- Technological Advancements: Partnering with tech companies to implement AI-driven diagnostic tools, telemedicine platforms, and wearable health devices.
- Operational Efficiency: Adopting lean management principles and agile methodologies from the private sector to optimise resource allocation and reduce waiting times.
- Research and Development: Collaborating with pharmaceutical companies and biotech firms to accelerate drug discovery and personalised medicine initiatives.
- Digital Infrastructure: Engaging IT giants to develop robust, interoperable health information systems and cybersecurity measures.
- Service Design: Utilising design thinking approaches from innovative companies to reimagine patient experiences and care pathways.
However, leveraging private sector innovation is not without its challenges. It requires careful navigation of regulatory frameworks, ethical considerations, and public perception. As a consultant who has worked on both sides of the public-private divide, I've observed that successful partnerships hinge on clear governance structures, aligned incentives, and transparent communication.
The NHS must become a 'permeable membrane' for innovation, allowing the best ideas from the private sector to flow in while maintaining its core principles of equity and universal access.
One of the most promising avenues for leveraging private sector innovation is through 'innovation hubs' or 'accelerators' within the NHS. These entities can act as bridges between the public healthcare system and private innovators, providing a controlled environment for testing and scaling new solutions. I've seen firsthand how such initiatives can dramatically reduce the time-to-market for healthcare innovations while ensuring they meet the specific needs of the NHS.
Another critical aspect is the development of a robust intellectual property (IP) framework that incentivises private sector participation while safeguarding public interests. This involves crafting agreements that allow companies to profit from their innovations while ensuring the NHS retains access to critical technologies and data. My experience in negotiating such agreements has shown that when done right, they can create a win-win scenario for all stakeholders.
Wardley Map Assessment
The NHS is well-positioned to leverage private sector innovations but needs to accelerate its adoption of emerging technologies and innovative methodologies. By focusing on strengthening its innovation management capabilities, fostering cross-sector collaborations, and strategically investing in key areas like AI and personalised medicine, the NHS can significantly enhance its ability to deliver cutting-edge, efficient healthcare services. The emphasis on Innovation Hubs, Sandbox Environments, and Cross-Sector Secondments provides a solid foundation for driving innovation, but there's a need to ensure these initiatives are closely aligned with the most promising emerging technologies. Prioritising cybersecurity and developing clear regulatory frameworks for new technologies will be crucial for managing risks associated with this innovation-driven transformation.
[View full Wardley Map report](markdown/wardley_map_reports/wardley_map_report_46_english_Leveraging Private Sector Innovation.md)
To fully capitalise on private sector innovation, the NHS must also cultivate an internal culture that is receptive to external ideas. This involves training healthcare professionals in innovation management, creating channels for frontline staff to engage with private sector partners, and establishing metrics that value innovative outcomes alongside traditional performance indicators.
- Innovation Scouts: Designate NHS staff to actively seek out and evaluate private sector innovations relevant to healthcare.
- Sandbox Environments: Create controlled testing grounds within NHS trusts for piloting private sector solutions.
- Innovation Vouchers: Provide NHS departments with resources to 'purchase' innovative solutions from approved private sector providers.
- Cross-Sector Secondments: Facilitate staff exchanges between the NHS and innovative companies to cross-pollinate ideas and practices.
- Innovation Challenges: Launch open competitions inviting private sector solutions to specific NHS problems, with pathways to implementation for winning ideas.
It's crucial to remember that leveraging private sector innovation is not about privatisation or compromising the core values of the NHS. Rather, it's about selectively adopting and adapting private sector strengths to enhance public healthcare delivery. As we move forward, the NHS must strike a delicate balance between embracing innovation and maintaining its commitment to equitable, universal care.
The future of healthcare lies not in choosing between public or private models, but in creating a symbiotic ecosystem where the best of both worlds can thrive for the benefit of patients and society.
In conclusion, leveraging private sector innovation represents a vital pathway for the NHS to address its current challenges and prepare for future demands. By fostering strategic partnerships, creating supportive infrastructures, and cultivating an innovation-friendly culture, the NHS can harness the dynamism of the private sector while reinforcing its position as a cornerstone of UK healthcare. As we continue to navigate this complex landscape, ongoing evaluation and adaptation of our approach will be key to ensuring that private sector innovation truly serves the public good.
Risk-Sharing Models in Healthcare Delivery
Risk-sharing models in healthcare delivery represent a pivotal approach to fostering effective public-private partnerships within the NHS. These models distribute financial and operational risks between public and private entities, aligning incentives to improve healthcare outcomes while managing costs. As an expert in NHS reform, I've observed that well-designed risk-sharing arrangements can drive innovation, enhance efficiency, and ultimately lead to better patient care.
At its core, risk-sharing in healthcare delivery involves the strategic allocation of financial, clinical, and operational risks among multiple stakeholders. This approach recognises that neither the public sector nor private entities can shoulder the entire burden of healthcare provision alone, especially given the complex challenges facing the NHS. By distributing risks, we create a shared responsibility for outcomes, encouraging all parties to work collaboratively towards common goals.
- Outcome-based contracts: Payments linked to specific health outcomes
- Capitation models: Fixed payments per patient, incentivising efficient care
- Gain-sharing agreements: Shared savings from cost reductions or improved outcomes
- Risk corridors: Limiting financial exposure for both public and private partners
- Performance bonds: Financial guarantees tied to meeting agreed-upon targets
Outcome-based contracts, for instance, have shown particular promise in areas such as elective surgeries and chronic disease management. By tying payments to specific health outcomes, these contracts incentivise private providers to focus on quality and effectiveness rather than volume of services. In my consultancy work, I've seen such contracts lead to significant improvements in patient outcomes and satisfaction, while also providing better value for money for the NHS.
Risk-sharing models are not just about financial arrangements; they're about creating a true partnership where both public and private entities are invested in the success of healthcare delivery. When implemented correctly, they can transform the way we approach healthcare challenges.
Capitation models, another form of risk-sharing, involve paying providers a fixed amount per patient, regardless of the actual services delivered. This approach encourages a focus on preventive care and efficient resource utilisation. However, it's crucial to design these models carefully to avoid unintended consequences such as undertreatment or cherry-picking of healthier patients. In my experience advising on such models, robust risk adjustment mechanisms and quality metrics are essential safeguards.
Gain-sharing agreements have proven effective in aligning incentives between the NHS and private partners. These arrangements allow both parties to share in the financial benefits resulting from improved efficiency or outcomes. For example, in a project I led involving orthopaedic services, a gain-sharing model led to a 15% reduction in length of stay and a 20% improvement in patient-reported outcomes, with the resulting savings shared between the NHS trust and the private provider.
Risk corridors and performance bonds are tools that can help manage the financial risks associated with public-private partnerships. Risk corridors limit the potential losses (and gains) for private partners, making participation more attractive while still maintaining incentives for performance. Performance bonds, on the other hand, provide financial guarantees that private partners will meet agreed-upon targets, offering protection for the NHS.
Wardley Map Assessment
The Wardley Map reveals a healthcare system in transition, with significant opportunities for innovation in risk-sharing models and data-driven decision-making. The strategic focus should be on accelerating the evolution of key components like Data Analytics and AI, while ensuring robust governance and public accountability. Success will depend on effectively managing the cultural shift and aligning incentives across the ecosystem. The integration of Value-based Healthcare principles and the development of advanced Risk-Sharing Models present significant opportunities for improving patient outcomes and system efficiency.
[View full Wardley Map report](markdown/wardley_map_reports/wardley_map_report_47_english_Risk-Sharing Models in Healthcare Delivery.md)
While risk-sharing models offer significant potential benefits, their implementation is not without challenges. One key consideration is the need for sophisticated data systems and analytics capabilities to accurately measure outcomes and allocate risks. Additionally, there must be a cultural shift within both the NHS and private sector partners towards true collaboration and shared accountability.
Transparency and public accountability are also crucial elements in successful risk-sharing arrangements. Clear communication about the nature of these partnerships, their objectives, and their outcomes is essential to maintain public trust in the NHS. In my role advising on public-private partnerships, I've consistently emphasised the importance of robust governance structures and regular public reporting to ensure accountability.
The success of risk-sharing models hinges on striking the right balance between incentivising innovation and protecting the core values of the NHS. It's about creating partnerships that enhance, rather than undermine, the principles of universal healthcare.
Looking ahead, the evolution of risk-sharing models in NHS partnerships will likely be shaped by advancements in data analytics, artificial intelligence, and value-based healthcare approaches. These technologies offer the potential for more nuanced risk assessment and outcome measurement, enabling increasingly sophisticated and effective risk-sharing arrangements.
In conclusion, risk-sharing models represent a powerful tool for enhancing public-private partnerships within the NHS. When thoughtfully designed and implemented, these models can drive innovation, improve efficiency, and ultimately lead to better health outcomes for patients. However, their success depends on careful planning, robust governance, and a genuine commitment to collaboration from all stakeholders involved. As we continue to navigate the complex landscape of NHS reform, risk-sharing models will undoubtedly play a crucial role in shaping the future of healthcare delivery in the UK.
Ensuring Public Accountability in Partnerships
As we delve into the critical aspect of ensuring public accountability in public-private partnerships (PPPs) within the NHS, it's essential to recognise the delicate balance between leveraging private sector expertise and maintaining the core values of a public healthcare system. The NHS, as a publicly funded institution, must uphold the highest standards of transparency, efficiency, and accountability in all its operations, including partnerships with private entities.
Public accountability in PPPs is not merely a regulatory requirement; it is a fundamental principle that underpins the trust between the NHS and the citizens it serves. As we explore this topic, we'll examine the multifaceted approaches to maintaining accountability, the challenges faced, and the innovative solutions being implemented across the healthcare landscape.
- Transparency in contract negotiations and terms
- Performance monitoring and reporting mechanisms
- Financial audits and value-for-money assessments
- Public consultation and stakeholder engagement
- Regulatory oversight and compliance frameworks
One of the primary mechanisms for ensuring accountability is through rigorous transparency in contract negotiations and terms. All PPP agreements should be subject to public scrutiny, with clear disclosure of financial arrangements, risk allocation, and performance targets. This level of openness not only fosters trust but also allows for informed public debate on the merits of such partnerships.
Transparency is the bedrock of public trust in healthcare partnerships. Without it, we risk eroding the very foundation of our national health service.
Performance monitoring and reporting mechanisms form another crucial pillar of accountability. These should be embedded within PPP contracts, with regular, publicly accessible reports on key performance indicators (KPIs). Such KPIs might include patient outcomes, waiting times, and financial efficiency metrics. It's vital that these metrics are not only quantitative but also qualitative, capturing the essence of patient care and satisfaction.
Financial audits and value-for-money assessments are indispensable tools in the accountability toolkit. Independent auditors should conduct regular reviews of PPP financial arrangements, ensuring that public funds are being used efficiently and effectively. These audits should go beyond mere compliance checks, delving into the true value delivered to the NHS and, by extension, to patients.
Public consultation and stakeholder engagement represent a proactive approach to accountability. Before entering into significant PPPs, the NHS should conduct thorough consultations with patients, healthcare professionals, and local communities. This not only ensures that partnerships align with public needs and expectations but also builds a sense of shared ownership and accountability.
Engaging the public in healthcare decisions isn't just good practice; it's a moral imperative. The NHS belongs to the people, and their voices must be heard in shaping its future.
Regulatory oversight and compliance frameworks provide the necessary structure for maintaining accountability. Bodies such as the Care Quality Commission (CQC) and NHS Improvement play crucial roles in setting standards, monitoring performance, and enforcing compliance. These regulatory mechanisms should be continuously evolved to address the unique challenges posed by PPPs, ensuring that private partners are held to the same high standards as public healthcare providers.
One innovative approach to enhancing accountability is the implementation of blockchain technology for contract management and performance tracking. This can provide an immutable, transparent record of all transactions and performance metrics, accessible to auditors and the public alike. Such technological solutions can significantly reduce the risk of data manipulation and enhance trust in PPP arrangements.
Wardley Map Assessment
The Wardley Map reveals a comprehensive approach to ensuring public accountability in NHS public-private partnerships, with a clear focus on maintaining public trust. While traditional accountability mechanisms are well-established, there are significant opportunities for innovation, particularly in leveraging emerging technologies like blockchain. The strategic focus should be on enhancing transparency, improving public engagement, and standardising processes across partnerships. By addressing identified gaps and embracing technological advancements, the NHS can create a more robust, transparent, and trustworthy system of public-private partnerships.
[View full Wardley Map report](markdown/wardley_map_reports/wardley_map_report_48_english_Ensuring Public Accountability in Partnerships.md)
Another critical aspect of ensuring accountability is the establishment of clear exit strategies and performance-based contract termination clauses. These provide the NHS with the necessary leverage to protect public interests if partnerships fail to deliver expected outcomes. Such clauses act as powerful incentives for private partners to maintain high standards of performance and accountability.
It's also crucial to consider the role of whistleblower protection in maintaining accountability. NHS staff and private sector employees involved in PPPs should feel empowered to report any misconduct or breaches of public trust without fear of reprisal. Robust whistleblower protection mechanisms are essential safeguards against potential abuses within partnership arrangements.
- Implement blockchain for transparent contract management
- Establish clear exit strategies and performance-based termination clauses
- Enhance whistleblower protection mechanisms
- Develop public-facing dashboards for real-time performance monitoring
- Create citizen oversight committees for major PPP projects
As we look to the future of PPPs in the NHS, it's clear that accountability mechanisms must evolve to keep pace with changing healthcare landscapes and technological advancements. The development of public-facing dashboards for real-time performance monitoring and the creation of citizen oversight committees for major PPP projects are just two examples of innovative approaches that could further enhance public accountability.
In the digital age, accountability should be as real-time and accessible as our healthcare services aspire to be. Technology can bridge the gap between complex partnerships and public understanding.
In conclusion, ensuring public accountability in NHS partnerships with the private sector is a complex but essential task. It requires a multi-faceted approach that combines traditional oversight mechanisms with innovative technologies and public engagement strategies. By maintaining a steadfast commitment to transparency, performance monitoring, and public involvement, the NHS can harness the benefits of private sector collaboration while upholding its core values and public service ethos. As we continue to navigate the challenges of healthcare reform, accountability will remain a cornerstone of public trust and the long-term success of the NHS.
International Collaboration and Knowledge Exchange
Learning from Global Best Practices
In the quest to revitalise the NHS, it is crucial to look beyond our borders and learn from global best practices in healthcare. The international healthcare landscape offers a wealth of innovative approaches, successful models, and valuable lessons that can inform and inspire the transformation of the NHS. By engaging in international collaboration and knowledge exchange, we can accelerate our progress, avoid reinventing the wheel, and adopt proven strategies that have yielded positive outcomes in other healthcare systems.
The NHS, despite its unique characteristics, faces challenges that are often universal in nature. Issues such as ageing populations, rising healthcare costs, workforce shortages, and the integration of new technologies are common across many developed nations. By studying how other countries have tackled these challenges, we can gain valuable insights and adapt successful solutions to the UK context.
- Comparative healthcare system analysis
- International benchmarking of health outcomes
- Collaborative research initiatives
- Exchange programmes for healthcare professionals
- Participation in global health forums and conferences
One of the most effective ways to learn from global best practices is through comparative healthcare system analysis. By examining the structures, funding models, and delivery mechanisms of high-performing healthcare systems in countries such as Sweden, Singapore, or Australia, we can identify elements that contribute to their success. For instance, Sweden's approach to integrated care for the elderly or Singapore's innovative health savings accounts could offer valuable lessons for the NHS.
As a senior health policy advisor notes, 'International benchmarking of health outcomes provides us with a clear picture of where we stand globally and helps us set ambitious yet achievable targets for improvement.'
Collaborative research initiatives play a crucial role in advancing healthcare knowledge and innovation. By participating in international research consortia, the NHS can contribute to and benefit from cutting-edge studies on topics such as precision medicine, health informatics, and population health management. These collaborations not only generate valuable insights but also foster relationships with leading institutions worldwide, creating opportunities for ongoing knowledge exchange.
Exchange programmes for healthcare professionals offer another powerful mechanism for learning from global best practices. By facilitating temporary placements or job swaps with healthcare systems in other countries, we can expose NHS staff to different approaches, technologies, and organisational cultures. This firsthand experience can spark innovation, challenge existing paradigms, and bring fresh perspectives to longstanding challenges within the NHS.
Wardley Map Assessment
The Wardley Map reveals a strategic focus on international knowledge exchange to address healthcare challenges faced by the NHS. While foundational components like the International Knowledge Exchange Unit are in place, there's significant opportunity to evolve the Culture of Openness and enhance dissemination mechanisms. By prioritising these areas and leveraging global partnerships, the NHS can significantly improve its ability to adopt best practices and innovate in healthcare delivery. The key to success lies in balancing short-term improvements in exchange mechanisms with long-term cultural and structural changes to fully embed international knowledge exchange into the NHS's operational DNA.
[View full Wardley Map report](markdown/wardley_map_reports/wardley_map_report_49_english_Learning from Global Best Practices.md)
Participation in global health forums and conferences is essential for staying abreast of international developments and emerging trends in healthcare. These events provide platforms for NHS leaders to engage with their counterparts from around the world, share experiences, and explore potential collaborations. They also offer opportunities to showcase NHS innovations and contribute to global discussions on pressing healthcare issues.
However, it is important to approach international best practices with a critical eye and a deep understanding of the local context. What works well in one country may not be directly transferable to the UK due to differences in culture, demographics, or healthcare system structures. The key is to identify the underlying principles that drive success and adapt them thoughtfully to the NHS environment.
A leading expert in healthcare innovation emphasises, 'The goal is not to copy other systems wholesale, but to learn, adapt, and innovate based on global insights, always keeping the unique strengths and challenges of the NHS in mind.'
To effectively harness global best practices, the NHS should establish a dedicated unit or team responsible for international knowledge exchange. This team would be tasked with systematically scanning the global healthcare landscape, identifying relevant innovations and successful models, and facilitating their evaluation and potential adoption within the NHS. They would also serve as a point of contact for international collaborations and ensure that insights gained are disseminated effectively throughout the organisation.
- Establish a dedicated international knowledge exchange unit
- Develop a framework for evaluating and adapting global best practices
- Create channels for disseminating international insights across the NHS
- Foster long-term partnerships with leading healthcare systems globally
- Encourage a culture of openness to international ideas and innovations
In conclusion, learning from global best practices through international collaboration and knowledge exchange is not just beneficial but essential for the NHS as it seeks to transform and meet the healthcare challenges of the 21st century. By actively engaging with the global healthcare community, the NHS can accelerate its innovation, improve its performance, and ultimately deliver better health outcomes for the people of the UK. The key lies in striking the right balance between learning from others and maintaining the core values and strengths that have made the NHS a beacon of universal healthcare worldwide.
Cross-Border Health Initiatives
Here's the content with necessary corrections for UK English:
Cross-border health initiatives encompass a wide range of collaborative efforts, including joint research projects, shared healthcare services, harmonisation of medical standards, and coordinated responses to health emergencies. For the NHS, engaging in such initiatives offers numerous opportunities to enhance its capabilities, learn from international best practices, and contribute to global health advancements.
- Collaborative Research and Development
- Shared Healthcare Services
- Harmonisation of Medical Standards
- Coordinated Emergency Response
- Health Workforce Mobility
- Digital Health Interoperability
One of the primary benefits of cross-border health initiatives is the acceleration of medical research and innovation. By pooling resources, expertise, and data across countries, the NHS can participate in large-scale studies that would be challenging to conduct within a single nation. This collaborative approach is particularly valuable in areas such as rare diseases, where patient populations in individual countries may be too small for meaningful research.
International collaboration in medical research has the potential to revolutionise our understanding of diseases and accelerate the development of new treatments. By working together across borders, we can achieve far more than any single country could on its own.
Another significant aspect of cross-border health initiatives is the potential for shared healthcare services. In regions with close geographical proximity, such as the UK and continental Europe, there are opportunities to optimise resource allocation and improve patient access to specialised treatments. For instance, the NHS could explore agreements with neighbouring countries to share specialised medical equipment or provide cross-border access to rare expertise, thereby enhancing the range of services available to patients while managing costs effectively.
Harmonisation of medical standards is another critical area where cross-border initiatives can drive improvements. By aligning clinical guidelines, quality standards, and regulatory frameworks with international best practices, the NHS can enhance the quality and consistency of care provided. This alignment also facilitates easier collaboration with international partners and can streamline processes for adopting innovative treatments and technologies developed abroad.
The COVID-19 pandemic has underscored the importance of coordinated international responses to health emergencies. Cross-border health initiatives play a vital role in establishing robust systems for early warning, data sharing, and collaborative crisis management. By actively participating in such initiatives, the NHS can strengthen its preparedness for future health emergencies and contribute to global health security.
The pandemic has taught us that health challenges do not respect national borders. Our ability to respond effectively to future crises depends on our willingness to work together across countries, sharing information and resources in real-time.
Health workforce mobility is another area where cross-border initiatives can benefit the NHS. By participating in international exchange programmes and fostering a more fluid movement of healthcare professionals across borders, the NHS can address skill shortages, promote knowledge transfer, and provide valuable development opportunities for its staff. However, this must be balanced with strategies to retain talent and ensure the sustainability of the domestic healthcare workforce.
Digital health interoperability is increasingly becoming a focus of cross-border health initiatives. As healthcare systems worldwide embrace digital transformation, there is a growing need for standardised approaches to health data exchange and interoperability of digital health systems. By engaging in international efforts to develop common standards and protocols, the NHS can ensure that its digital health infrastructure remains at the forefront of global advancements and can seamlessly interact with systems in other countries.
Wardley Map Assessment
The map reveals a strategic focus on leveraging cross-border health initiatives to enhance the NHS's capabilities in addressing global health challenges. Key areas for development include digital health interoperability, workforce mobility, and cultural competency. The strategy should prioritise these areas while ensuring robust legal and ethical frameworks are in place. The evolving nature of many components suggests a dynamic environment that requires continuous adaptation and innovation. By fostering international partnerships and focusing on shared healthcare services, the NHS can position itself as a leader in global health collaboration.
[View full Wardley Map report](markdown/wardley_map_reports/wardley_map_report_50_english_Cross-Border Health Initiatives.md)
Implementing effective cross-border health initiatives requires careful consideration of legal, ethical, and practical challenges. Issues such as data protection, patient privacy, and differences in healthcare systems and cultural contexts must be addressed. The NHS will need to develop robust frameworks for international collaboration that protect patient interests while maximising the benefits of cross-border initiatives.
- Develop clear legal and ethical frameworks for cross-border collaboration
- Establish mechanisms for secure and compliant data sharing
- Create dedicated teams to manage international partnerships
- Invest in language and cultural competency training for staff
- Regularly assess the impact and value of cross-border initiatives
- Ensure alignment with NHS core principles and objectives
In conclusion, cross-border health initiatives offer significant potential for the NHS to enhance its capabilities, drive innovation, and improve patient care. By actively engaging in international collaboration and knowledge exchange, the NHS can leverage global expertise and resources to address its challenges more effectively. As we look to revitalise the NHS, embracing cross-border health initiatives should be seen as a key strategy for fostering innovation, improving efficiency, and ultimately delivering better health outcomes for the UK population.
Collaborative Research and Development
In the realm of healthcare innovation, collaborative research and development (R&D) stands as a cornerstone for advancing medical knowledge, improving patient outcomes, and addressing global health challenges. As we seek to revitalise the NHS, fostering international partnerships in R&D becomes not just beneficial, but essential. This approach allows the NHS to tap into a global pool of expertise, share resources, and accelerate the pace of innovation in ways that would be impossible in isolation.
The NHS, with its vast patient population and comprehensive health data, is uniquely positioned to contribute to and benefit from international R&D collaborations. By engaging in these partnerships, the NHS can leverage its strengths while addressing its challenges, ultimately enhancing its capacity to deliver cutting-edge, evidence-based care to patients across the UK.
- Establishing Global Research Networks
- Sharing Data and Resources
- Collaborative Clinical Trials
- Joint Technology Development
- Policy and Regulatory Harmonisation
Establishing Global Research Networks is a crucial first step in fostering collaborative R&D. These networks bring together researchers, clinicians, and institutions from around the world, creating a platform for knowledge exchange and joint problem-solving. For the NHS, participation in such networks can provide access to diverse patient populations, innovative research methodologies, and cutting-edge technologies that may not be available within the UK alone.
Global research networks are the lifeblood of modern medical innovation. They allow us to tackle complex health challenges with a collective intelligence that transcends national boundaries.
Sharing Data and Resources is another critical aspect of collaborative R&D. The NHS's comprehensive health records represent a goldmine of data that, when shared responsibly and ethically, can drive significant advancements in medical research. By participating in international data-sharing initiatives, the NHS can contribute to and benefit from large-scale studies on disease patterns, treatment efficacy, and population health trends. However, this must be balanced with robust data protection measures to ensure patient privacy and maintain public trust.
Collaborative Clinical Trials offer a powerful mechanism for accelerating the development and validation of new treatments. By participating in multi-centre, international clinical trials, the NHS can provide its patients with early access to promising therapies while contributing to the global evidence base. This approach is particularly valuable for rare diseases or complex conditions where patient recruitment can be challenging within a single country.
Joint Technology Development initiatives allow the NHS to collaborate with international partners in creating innovative healthcare solutions. This could range from developing new medical devices and diagnostic tools to creating advanced AI algorithms for disease prediction and management. By pooling resources and expertise, these collaborations can reduce development costs, mitigate risks, and accelerate the path from concept to clinical application.
In the rapidly evolving landscape of healthcare technology, no single organisation or country can go it alone. International collaboration is not just beneficial; it's imperative for staying at the forefront of medical innovation.
Policy and Regulatory Harmonisation is a crucial enabler of effective international R&D collaboration. By working with international partners to align research protocols, ethical standards, and regulatory frameworks, the NHS can help create a more conducive environment for cross-border collaboration. This harmonisation can streamline the process of conducting multi-national studies, facilitate the sharing of research findings, and accelerate the adoption of proven innovations across different healthcare systems.
However, collaborative R&D is not without its challenges. Differences in regulatory environments, intellectual property laws, and cultural approaches to healthcare can create obstacles. Moreover, ensuring equitable partnerships that benefit all parties involved requires careful negotiation and clear governance structures. The NHS must navigate these complexities while maintaining its commitment to public service and universal healthcare principles.
Wardley Map Assessment
The Wardley Map reveals a strategic position poised for significant advancement in international healthcare R&D collaboration. The NHS, leveraging its central role and strong partnerships, has the opportunity to lead global efforts in data sharing, collaborative research, and technology development. Key to success will be addressing regulatory harmonisation and data protection challenges, while fostering innovation in emerging technologies. By prioritising these areas, the NHS can enhance its global influence, accelerate research outcomes, and ultimately improve patient care on an international scale.
[View full Wardley Map report](markdown/wardley_map_reports/wardley_map_report_51_english_Collaborative Research and Development.md)
In conclusion, collaborative research and development represents a powerful tool for the NHS to enhance its capabilities, address its challenges, and contribute to global health advancements. By actively engaging in international partnerships, the NHS can accelerate innovation, improve patient care, and strengthen its position as a world-leading healthcare system. As we chart the course for a revitalised NHS, embracing and expanding these collaborative efforts must be a key priority, ensuring that the benefits of global medical progress are swiftly translated into improved health outcomes for patients across the UK.
Conclusion: A Roadmap for NHS Transformation
Key Takeaways and Action Points
Prioritizing Reform Initiatives
As we conclude our comprehensive analysis of the NHS and its path to revitalisation, it is crucial to distil our findings into actionable insights and prioritise reform initiatives. The complexity of the NHS system demands a strategic approach to change, one that balances urgency with feasibility and impact. Drawing from our extensive examination of the challenges and opportunities facing the NHS, we can now outline key takeaways and action points that will form the foundation of a transformative roadmap.
Effective reform of the NHS requires a delicate balance between bold vision and pragmatic implementation. We must be ambitious in our goals, yet meticulous in our execution.
To prioritise reform initiatives effectively, we must consider several critical factors: the potential impact on patient outcomes, the feasibility of implementation given current resources and constraints, the alignment with core NHS values, and the long-term sustainability of proposed changes. With these considerations in mind, we can identify the following key takeaways and action points:
- Embrace data-driven decision making as a cornerstone of NHS reform
- Invest in workforce development and well-being as a priority
- Accelerate the adoption of digital health technologies
- Redesign care pathways with a focus on patient-centricity and integration
- Develop sustainable funding models that incentivise value-based care
- Foster cross-sector collaborations to address complex health challenges
Let us examine each of these priorities in more detail, outlining specific action points for implementation:
- Embrace data-driven decision making: The NHS must prioritise the development of robust health informatics systems and cultivate a culture of data literacy among staff. Action points include:
- Establish a centralised data governance framework to ensure data quality and interoperability
- Implement advanced analytics platforms for predictive modelling and resource allocation
- Provide comprehensive data literacy training programmes for all levels of NHS staff
- Invest in workforce development and well-being: Addressing staff shortages and burnout is critical for the NHS's future. Key actions include:
- Develop innovative recruitment strategies to attract and retain healthcare professionals
- Implement comprehensive mental health support programmes for NHS staff
- Create clear career progression pathways and continuous professional development opportunities
- Accelerate the adoption of digital health technologies: Leveraging technology can significantly improve efficiency and access to care. Priority actions include:
- Scale up telemedicine services across all appropriate care settings
- Invest in AI and machine learning technologies for diagnostics and care planning
- Implement a secure, interoperable electronic health record system across the NHS
- Redesign care pathways with a focus on patient-centricity and integration: Improving patient experience and outcomes requires a holistic approach to care. Key actions include:
- Develop integrated care models that seamlessly combine health and social care services
- Implement shared decision-making tools and processes across all patient interactions
- Establish community health hubs to promote preventive care and manage chronic conditions
- Develop sustainable funding models that incentivise value-based care: Ensuring the long-term financial sustainability of the NHS is crucial. Priority actions include:
- Explore alternative financing mechanisms, such as social impact bonds for health outcomes
- Implement value-based payment models that reward quality and efficiency
- Develop long-term financial forecasting tools to anticipate and plan for future healthcare demands
- Foster cross-sector collaborations to address complex health challenges: Leveraging expertise and resources across sectors can drive innovation and improve outcomes. Key actions include:
- Establish formal partnerships between the NHS, academia, and private sector for research and innovation
- Create collaborative platforms for knowledge exchange with international healthcare systems
- Develop joint commissioning frameworks between health and social care organisations
By focusing on these priority areas and implementing the associated action points, the NHS can embark on a transformative journey towards a more resilient, efficient, and patient-centred healthcare system. However, it is important to recognise that these initiatives are interconnected and mutually reinforcing. Success in one area will often depend on and contribute to progress in others.
The path to NHS reform is not a series of isolated changes, but a carefully orchestrated symphony of interconnected initiatives. Each action we take must harmonise with the others to create a truly transformative impact.
As we move forward with these priority reforms, it will be essential to establish clear metrics for success, regularly assess progress, and remain adaptable in the face of emerging challenges and opportunities. The journey of NHS transformation is ongoing, and these key takeaways and action points provide a robust foundation for sustainable, impactful change.
Wardley Map Assessment
This Wardley Map reveals a comprehensive approach to NHS transformation, with a clear focus on improving patient outcomes through technological innovation, workforce development, and system-wide collaboration. The strategic positioning of components suggests a forward-thinking approach, but also highlights areas requiring accelerated development, particularly in funding models and cross-sector collaborations. To succeed, the NHS should prioritise initiatives that address these gaps while continuing to leverage its strengths in data-driven decision making and digital health technologies. The evolving nature of key components underscores the need for adaptability and continuous innovation in the face of a rapidly changing healthcare landscape.
[View full Wardley Map report](markdown/wardley_map_reports/wardley_map_report_52_english_Prioritizing Reform Initiatives.md)
Overcoming Implementation Challenges
As we conclude our comprehensive analysis of revitalising the NHS, it is crucial to address the formidable task of overcoming implementation challenges. The road to transforming a complex, nationwide healthcare system is fraught with obstacles, but with strategic planning and unwavering commitment, these challenges can be surmounted.
One of the primary hurdles in implementing large-scale changes within the NHS is the inherent resistance to change that exists within any established institution. This resistance can stem from various sources, including entrenched practices, fear of the unknown, and concerns about job security. To overcome this, a multi-faceted approach is necessary.
- Develop a clear and compelling vision for change
- Engage stakeholders at all levels in the change process
- Provide comprehensive training and support for new systems and processes
- Implement changes incrementally to build confidence and demonstrate success
- Establish robust communication channels to address concerns and share progress
Another significant challenge is the need for substantial financial investment to implement many of the proposed reforms, particularly in areas such as digital transformation and workforce development. In an era of fiscal constraints, securing the necessary funding requires innovative approaches and a clear demonstration of return on investment.
- Develop detailed business cases for each major initiative
- Explore public-private partnerships to share costs and risks
- Prioritise investments based on potential impact and feasibility
- Implement rigorous cost-benefit analyses and performance metrics
- Leverage existing resources more efficiently through process optimisation
The path to transforming the NHS is not about wholesale dismantling and rebuilding, but rather about strategic evolution that preserves what works while boldly innovating where necessary.
The complexity of the NHS system itself presents a formidable implementation challenge. With its myriad interconnected departments, diverse workforce, and varied stakeholders, coordinating change across the entire organisation requires meticulous planning and execution.
- Establish a dedicated transformation office to oversee and coordinate change initiatives
- Develop a detailed implementation roadmap with clear milestones and responsibilities
- Create cross-functional teams to address interdependencies and ensure alignment
- Implement robust project management methodologies to track progress and manage risks
- Regularly review and adjust implementation strategies based on feedback and outcomes
Cultural change within the NHS is perhaps one of the most challenging aspects of implementation. Shifting mindsets from traditional models of healthcare delivery to more patient-centric, data-driven approaches requires sustained effort and leadership.
- Lead by example, with senior leadership visibly championing the change
- Celebrate early wins and showcase success stories to build momentum
- Embed new values and practices in performance management and reward systems
- Provide opportunities for staff to contribute ideas and shape the change process
- Invest in leadership development to equip managers with change management skills
Successful transformation of the NHS is not just about systems and processes; it's about winning hearts and minds, and creating a culture that embraces continuous improvement and innovation.
Lastly, the political landscape surrounding the NHS can present significant implementation challenges. With the NHS being a cornerstone of British society, any major changes are likely to face intense scrutiny and potential opposition from various quarters.
- Develop a comprehensive stakeholder engagement strategy
- Build cross-party support for key initiatives to ensure continuity
- Engage patient groups and the public in the change process to build trust
- Maintain transparency in decision-making and progress reporting
- Be prepared to adapt plans in response to legitimate concerns and feedback
Wardley Map Assessment
The Wardley Map presents a comprehensive view of the challenges and strategies for NHS transformation. It highlights the complexity of the task and the need for a multi-faceted approach. The key to success lies in addressing resistance to change, securing adequate financial investment, and managing the complex interplay of cultural, political, and systemic factors. The map suggests a strong foundation in terms of strategic planning but indicates the need for focused effort on execution, particularly in change management and stakeholder engagement. The transformation office and implementation roadmap will be critical in coordinating these efforts and driving the overall transformation process.
[View full Wardley Map report](markdown/wardley_map_reports/wardley_map_report_53_english_Overcoming Implementation Challenges.md)
By acknowledging these implementation challenges and proactively developing strategies to address them, we can significantly increase the likelihood of successful NHS transformation. The journey ahead is undoubtedly complex, but with careful planning, strong leadership, and a commitment to continuous learning and adaptation, the vision of a revitalised NHS can become a reality.
Measuring Progress and Impact
As we conclude our comprehensive blueprint for revitalising the NHS, it is crucial to establish robust mechanisms for measuring progress and impact. This final subsection serves as a critical bridge between the strategies we've outlined and their practical implementation, ensuring that our efforts to transform the NHS are both measurable and accountable.
Effective measurement of progress and impact is not merely about collecting data; it's about fostering a culture of continuous improvement and evidence-based decision-making within the NHS. By implementing a comprehensive framework for evaluation, we can ensure that reforms are delivering tangible benefits to patients, staff, and the broader healthcare system.
What gets measured gets managed. In the context of NHS transformation, this means creating a clear line of sight between our strategic objectives and the outcomes we achieve on the ground.
To effectively measure progress and impact, we must consider both quantitative and qualitative metrics. Quantitative measures provide us with hard data on performance improvements, while qualitative assessments offer insights into the lived experiences of patients and healthcare professionals. This balanced approach ensures we capture the full spectrum of impact across the NHS.
- Key Performance Indicators (KPIs): Develop a set of comprehensive KPIs that align with the strategic objectives outlined in our transformation plan. These should cover areas such as patient outcomes, operational efficiency, staff satisfaction, and financial sustainability.
- Regular Reporting Cycles: Establish a consistent reporting schedule to track progress against KPIs. This could involve monthly operational reports, quarterly strategic reviews, and annual comprehensive assessments.
- Stakeholder Feedback Mechanisms: Implement robust systems for gathering feedback from patients, staff, and other stakeholders. This could include patient satisfaction surveys, staff engagement polls, and community health forums.
- Independent Audits: Commission regular independent audits to provide an objective assessment of progress and identify areas for improvement.
- Data Analytics Capabilities: Invest in advanced data analytics tools and capabilities to process and interpret the vast amount of data generated across the NHS, enabling more nuanced and timely insights.
One of the most critical aspects of measuring progress and impact is ensuring that the insights gained are translated into actionable improvements. This requires a clear governance structure and decision-making process that can respond swiftly to emerging trends and challenges identified through our measurement framework.
The true measure of success in NHS transformation is not just in the metrics we track, but in our ability to use those insights to drive continuous improvement and deliver better outcomes for patients.
It's also important to recognise that measuring progress and impact in a system as complex as the NHS is not without its challenges. We must be prepared to refine our measurement approaches as we learn and adapt. This might involve adjusting KPIs, introducing new data collection methods, or recalibrating our benchmarks as the healthcare landscape evolves.
- Balancing Short-term and Long-term Metrics: Ensure our measurement framework captures both immediate improvements and long-term systemic changes.
- Addressing Data Quality Issues: Implement rigorous data governance practices to ensure the accuracy and reliability of the information we're using to measure progress.
- Avoiding Perverse Incentives: Carefully design metrics to prevent unintended consequences or gaming of the system.
- Communicating Progress Effectively: Develop clear and accessible ways of communicating progress to all stakeholders, from policymakers to the general public.
- Benchmarking Against International Standards: Regularly compare NHS performance against international best practices to drive continuous improvement.
By embedding a robust approach to measuring progress and impact throughout our NHS transformation journey, we create a virtuous cycle of improvement. Each insight gained becomes an opportunity to refine our strategies, allocate resources more effectively, and ultimately deliver better care to patients across the UK.
Wardley Map Assessment
The NHS Transformation Measurement Framework provides a solid foundation for driving and tracking improvements in healthcare delivery. However, to fully realise its potential, the NHS needs to focus on evolving its supporting processes, particularly in data analytics, governance, and continuous improvement methodologies. By addressing these areas and fostering a culture of data-driven decision-making and ongoing adaptation, the NHS can enhance its ability to deliver high-quality, efficient, and sustainable healthcare services that meet the evolving needs of its stakeholders.
[View full Wardley Map report](markdown/wardley_map_reports/wardley_map_report_54_english_Measuring Progress and Impact.md)
As we move forward with implementing the comprehensive blueprint outlined in this book, let us remember that measuring progress and impact is not an afterthought, but an integral part of the transformation process itself. It is through diligent measurement, analysis, and adaptation that we will realise our vision of a revitalised NHS – one that is more efficient, more responsive, and better equipped to meet the healthcare challenges of the 21st century.
The Future of Healthcare in the UK
Envisioning a Resilient and Adaptive NHS
As we look towards the future of healthcare in the UK, it is crucial to envision an NHS that is not only resilient in the face of challenges but also adaptive to the rapidly evolving landscape of medical science, technology, and societal needs. The NHS of tomorrow must be built on the solid foundation of its core principles while embracing innovation and flexibility to meet the changing demands of the population it serves.
A resilient and adaptive NHS will be characterised by several key attributes that will enable it to thrive in an uncertain future:
- Agile organisational structures that can quickly respond to emerging health crises
- Robust digital infrastructure supporting seamless data sharing and analysis
- A culture of continuous learning and innovation among healthcare professionals
- Sustainable funding models that balance long-term planning with short-term flexibility
- Strong partnerships across public, private, and third sectors to leverage diverse expertise
To achieve this vision, the NHS must undergo a transformative journey that touches every aspect of its operations. This transformation will require a delicate balance between preserving the core values that have made the NHS a beacon of universal healthcare and embracing radical changes necessary for its future sustainability.
The NHS of the future will not just be a healthcare provider, but a proactive partner in the nation's health, leveraging data and technology to predict and prevent illness before it occurs.
One of the most significant shifts we can anticipate is the move towards predictive and preventative care. By harnessing the power of big data, artificial intelligence, and genomics, the NHS will be able to identify health risks at a population and individual level, allowing for targeted interventions before conditions become critical. This approach not only improves patient outcomes but also helps to manage resources more effectively.
Another crucial aspect of the future NHS will be its ability to deliver personalised medicine. As our understanding of genetics and individual health profiles deepens, treatments will become increasingly tailored to each patient's unique needs. This personalisation extends beyond clinical care to encompass lifestyle factors, mental health, and social determinants of health, creating a holistic approach to wellbeing.
Wardley Map Assessment
The Wardley Map reveals a strategic vision for an NHS that is evolving towards a more proactive, personalised, and digitally-enabled healthcare system. Key to success will be the effective development of digital infrastructure, workforce capabilities, and innovative care models, balanced with sustainable funding approaches. The NHS has the potential to lead global healthcare innovation, but must navigate significant transformational challenges to realise this vision.
[View full Wardley Map report](markdown/wardley_map_reports/wardley_map_report_55_english_Envisioning a Resilient and Adaptive NHS.md)
The workforce of the future NHS will be markedly different from today's. We can expect to see new roles emerging at the intersection of healthcare and technology, such as clinical data scientists and AI ethics officers. Traditional roles will evolve, with healthcare professionals becoming adept at using advanced technologies to augment their clinical decision-making. Continuous learning and upskilling will be embedded into the fabric of NHS culture, ensuring that the workforce remains at the cutting edge of medical practice.
In the NHS of tomorrow, every healthcare professional will be a lifelong learner, constantly adapting their skills to harness new technologies and deliver the best possible care to patients.
The physical infrastructure of the NHS will also undergo significant changes. While centralised hospitals will continue to play a crucial role in delivering complex and emergency care, we can expect to see a shift towards community-based care settings. These local health hubs will integrate primary care, specialist services, and social care, providing a one-stop-shop for most health needs. Telemedicine and remote monitoring technologies will enable many patients to receive high-quality care from the comfort of their homes, reducing the strain on physical infrastructure.
Sustainability will be at the heart of the future NHS, both in terms of environmental impact and financial viability. The healthcare sector will need to lead by example in reducing its carbon footprint, adopting green technologies, and promoting sustainable practices. Financially, the NHS will need to explore innovative funding models that can withstand economic fluctuations and demographic changes. This may include outcomes-based commissioning, social impact bonds, and greater integration of health and social care budgets.
- Development of 'smart' hospitals and clinics that optimise resource use and patient flow
- Implementation of circular economy principles in medical supply chains
- Adoption of value-based healthcare models that prioritise patient outcomes over volume of services
- Creation of health innovation hubs to accelerate the development and adoption of new technologies
- Establishment of cross-sector partnerships to address wider determinants of health
The future NHS will also need to be prepared for global health challenges, including pandemics, antimicrobial resistance, and the health impacts of climate change. This will require robust surveillance systems, rapid response capabilities, and strong international collaborations. The lessons learned from the COVID-19 pandemic will be invaluable in shaping these preparedness strategies.
Ultimately, the success of this vision for a resilient and adaptive NHS will depend on the engagement and support of the British public. As the NHS evolves, it must maintain its position as a cherished national institution, adapting to new realities while staying true to its founding principle of providing care free at the point of use, based on clinical need rather than ability to pay.
The NHS of the future will be a dynamic, learning organisation that continuously evolves to meet the changing needs of the population, while remaining true to its core mission of providing equitable, high-quality healthcare for all.
By embracing this vision of a resilient and adaptive NHS, we can ensure that this vital institution not only survives but thrives in the face of future challenges, continuing to serve as a model of excellence in healthcare delivery for generations to come.
The Role of Citizens in Shaping Healthcare
As we envision the future of healthcare in the UK, it is crucial to recognise the pivotal role that citizens play in shaping the NHS. The traditional model of healthcare delivery, where patients were passive recipients of care, is rapidly evolving into a more collaborative and participatory system. This shift is not only necessary but essential for the long-term sustainability and effectiveness of the NHS.
Citizens are increasingly becoming active participants in their own health management, driven by advancements in technology, increased access to information, and a growing emphasis on preventive care. This transformation is reshaping the healthcare landscape in several key ways:
- Shared decision-making: Patients are now more involved in treatment decisions, working alongside healthcare professionals to determine the best course of action based on medical evidence and personal preferences.
- Digital health engagement: The proliferation of health apps, wearable devices, and online platforms is enabling citizens to monitor their health, access medical information, and engage with healthcare services more proactively.
- Community health initiatives: Local communities are taking a more active role in promoting health and wellbeing, from organising fitness programmes to supporting mental health awareness campaigns.
- Patient feedback and co-design: Healthcare services are increasingly seeking patient input in the design and improvement of services, recognising the value of lived experience in shaping effective care pathways.
- Health literacy and education: There is a growing focus on improving public understanding of health issues, empowering citizens to make informed decisions about their lifestyle and healthcare choices.
The empowerment of citizens in healthcare is not without its challenges. As a senior NHS official noted, 'We must strike a delicate balance between encouraging patient autonomy and ensuring that professional medical expertise remains at the core of healthcare delivery.' This balance is crucial to maintain the integrity and effectiveness of the NHS while harnessing the benefits of citizen engagement.
To fully realise the potential of citizen involvement in shaping healthcare, several key areas require attention:
- Digital inclusion: Ensuring that all segments of society, regardless of age, socioeconomic status, or digital literacy, can access and benefit from digital health tools and information.
- Health education: Developing comprehensive programmes to improve health literacy across all age groups, enabling citizens to make informed decisions about their health and healthcare.
- Patient representation: Strengthening mechanisms for patient voices to be heard at all levels of NHS decision-making, from local service design to national policy formulation.
- Collaborative care models: Developing and implementing care models that facilitate true partnership between healthcare professionals and patients, particularly for the management of chronic conditions.
- Data ownership and privacy: Addressing concerns around health data ownership, usage, and privacy to build trust and encourage citizen participation in data-driven healthcare initiatives.
The future of the NHS lies not just in the hands of policymakers and healthcare professionals, but in the active engagement of every citizen in their own health and the health of their communities.
As we look to the future, the role of citizens in shaping healthcare will undoubtedly continue to grow. The NHS must adapt to this new reality, embracing the opportunities it presents while addressing the challenges it poses. By fostering a culture of collaboration, empowerment, and shared responsibility, we can create a healthcare system that is not only more responsive to the needs of individuals and communities but also more resilient and sustainable in the face of future challenges.
Wardley Map Assessment
The Wardley Map reveals a NHS in transition, moving towards a more digitally-enabled, citizen-centric model of care. The strategic focus should be on accelerating digital transformation while ensuring inclusivity, maintaining trust through robust data governance, and fostering innovation in collaborative care models. Success will depend on effectively balancing rapid technological advancement with the need for equitable access and personalised care delivery.
[View full Wardley Map report](markdown/wardley_map_reports/wardley_map_report_56_english_The Role of Citizens in Shaping Healthcare.md)
The transformation towards a more citizen-centric NHS will require significant changes in organisational culture, service design, and policy frameworks. It will necessitate investment in digital infrastructure, training for healthcare professionals in collaborative care approaches, and the development of new metrics to measure the impact of citizen engagement on health outcomes and system efficiency.
Ultimately, the success of this transformation will depend on the willingness of all stakeholders – from policymakers and healthcare professionals to patients and community leaders – to embrace a new paradigm of healthcare delivery. One where the boundaries between service providers and service users are increasingly blurred, and where the collective wisdom and efforts of all citizens contribute to the health and wellbeing of the nation.
In the NHS of the future, every citizen will be both a beneficiary of healthcare services and a contributor to the health of the nation. This shift from a transactional to a participatory model of healthcare is not just desirable – it is essential for the long-term sustainability of our beloved National Health Service.
Preparing for Future Health Challenges
As we look towards the future of healthcare in the UK, it is imperative that the NHS positions itself to effectively respond to emerging health challenges. This forward-thinking approach requires a combination of strategic planning, technological innovation, and adaptive policies that can withstand the test of time and unforeseen circumstances.
One of the primary considerations in preparing for future health challenges is the changing demographic landscape of the UK. With an ageing population and increasing life expectancy, the NHS must gear up to handle a surge in age-related health issues, chronic conditions, and complex care needs. This demographic shift necessitates a reimagining of healthcare delivery models, with a greater emphasis on long-term care, home-based services, and integrated health and social care approaches.
The NHS of tomorrow must be built on the foundation of population health management, leveraging data and predictive analytics to anticipate and mitigate health risks before they become crises.
Climate change and environmental factors present another set of challenges that the NHS must prepare for. The health impacts of global warming, including the spread of new infectious diseases, increased respiratory issues due to air pollution, and mental health effects of climate-related disasters, require the NHS to develop robust environmental health strategies. This includes building resilient healthcare infrastructure, implementing sustainable practices within the health service, and collaborating with environmental agencies to address health determinants.
- Developing early warning systems for climate-related health risks
- Investing in research on climate-resilient healthcare practices
- Integrating environmental health considerations into all NHS policies and operations
- Collaborating with global health organisations to address transnational health threats
The rapid pace of technological advancement presents both opportunities and challenges for the future of healthcare. The NHS must stay at the forefront of medical innovations, such as personalised medicine, gene therapies, and AI-driven diagnostics. However, it must also navigate the ethical, legal, and social implications of these technologies. This requires a proactive approach to regulation, robust governance frameworks, and ongoing dialogue with the public about the role of technology in healthcare.
Another critical aspect of preparing for future health challenges is building a flexible and adaptable workforce. The NHS must invest in continuous professional development, cross-disciplinary training, and skills that may not yet be fully defined but will be crucial in the coming decades. This includes fostering a culture of innovation and lifelong learning among healthcare professionals, as well as developing new roles that bridge traditional healthcare with emerging fields such as data science and biotechnology.
The healthcare workforce of the future must be as dynamic and evolving as the challenges it faces. We need to create a learning health system that can rapidly adapt to new knowledge and changing circumstances.
Pandemic preparedness remains a critical consideration in light of recent global experiences. The NHS must institutionalise the lessons learned from COVID-19, enhancing its capacity for rapid response, scalable interventions, and effective public health communications. This includes maintaining strategic reserves of essential supplies, developing flexible care models that can quickly pivot during crises, and strengthening partnerships with research institutions for rapid vaccine and treatment development.
Wardley Map Assessment
The NHS is positioned to lead in addressing future health challenges, but success will require significant evolution in key areas. Priorities should include accelerating technological adoption, enhancing global collaboration, and developing innovative models for sustainable healthcare delivery. The integration of health and social care, coupled with a strong focus on environmental health and pandemic preparedness, will be crucial. To succeed, the NHS must foster an innovation culture, invest in workforce development, and leverage data-driven approaches to population health management.
[View full Wardley Map report](markdown/wardley_map_reports/wardley_map_report_57_english_Preparing for Future Health Challenges.md)
Financial sustainability in the face of these future challenges is paramount. The NHS must explore innovative funding models, such as outcomes-based commissioning and social impact bonds, which align financial incentives with long-term health outcomes. Additionally, investing in preventive care and public health initiatives can help mitigate future health burdens and associated costs.
Lastly, the NHS must embrace a global perspective in preparing for future health challenges. International collaboration in research, sharing of best practices, and coordinated responses to global health threats will be essential. The UK has the opportunity to position itself as a leader in global health innovation, leveraging its strengths in research, technology, and healthcare delivery to contribute to and benefit from international efforts to address future health challenges.
- Establishing international research consortia for emerging health threats
- Developing cross-border health information sharing systems
- Participating in global health governance forums and policy-making
- Creating exchange programmes for healthcare professionals to gain international experience
In conclusion, preparing for future health challenges requires the NHS to be proactive, innovative, and adaptable. By anticipating demographic shifts, embracing technological advancements, building a flexible workforce, and fostering global collaboration, the NHS can position itself to not only respond to future health challenges but to lead the way in shaping a healthier future for the UK and beyond.
Appendix: Further Reading on Wardley Mapping
The following books, primarily authored by Mark Craddock, offer comprehensive insights into various aspects of Wardley Mapping:
Core Wardley Mapping Series
-
Wardley Mapping, The Knowledge: Part One, Topographical Intelligence in Business
- Author: Simon Wardley
- Editor: Mark Craddock
- Part of the Wardley Mapping series (5 books)
- Available in Kindle Edition
- Amazon Link
This foundational text introduces readers to the Wardley Mapping approach:
- Covers key principles, core concepts, and techniques for creating situational maps
- Teaches how to anchor mapping in user needs and trace value chains
- Explores anticipating disruptions and determining strategic gameplay
- Introduces the foundational doctrine of strategic thinking
- Provides a framework for assessing strategic plays
- Includes concrete examples and scenarios for practical application
The book aims to equip readers with:
- A strategic compass for navigating rapidly shifting competitive landscapes
- Tools for systematic situational awareness
- Confidence in creating strategic plays and products
- An entrepreneurial mindset for continual learning and improvement
-
Wardley Mapping Doctrine: Universal Principles and Best Practices that Guide Strategic Decision-Making
- Author: Mark Craddock
- Part of the Wardley Mapping series (5 books)
- Available in Kindle Edition
- Amazon Link
This book explores how doctrine supports organizational learning and adaptation:
- Standardisation: Enhances efficiency through consistent application of best practices
- Shared Understanding: Fosters better communication and alignment within teams
- Guidance for Decision-Making: Offers clear guidelines for navigating complexity
- Adaptability: Encourages continuous evaluation and refinement of practices
Key features:
- In-depth analysis of doctrine's role in strategic thinking
- Case studies demonstrating successful application of doctrine
- Practical frameworks for implementing doctrine in various organizational contexts
- Exploration of the balance between stability and flexibility in strategic planning
Ideal for:
- Business leaders and executives
- Strategic planners and consultants
- Organizational development professionals
- Anyone interested in enhancing their strategic decision-making capabilities
-
Wardley Mapping Gameplays: Transforming Insights into Strategic Actions
- Author: Mark Craddock
- Part of the Wardley Mapping series (5 books)
- Available in Kindle Edition
- Amazon Link
This book delves into gameplays, a crucial component of Wardley Mapping:
- Gameplays are context-specific patterns of strategic action derived from Wardley Maps
- Types of gameplays include:
- User Perception plays (e.g., education, bundling)
- Accelerator plays (e.g., open approaches, exploiting network effects)
- De-accelerator plays (e.g., creating constraints, exploiting IPR)
- Market plays (e.g., differentiation, pricing policy)
- Defensive plays (e.g., raising barriers to entry, managing inertia)
- Attacking plays (e.g., directed investment, undermining barriers to entry)
- Ecosystem plays (e.g., alliances, sensing engines)
Gameplays enhance strategic decision-making by:
- Providing contextual actions tailored to specific situations
- Enabling anticipation of competitors' moves
- Inspiring innovative approaches to challenges and opportunities
- Assisting in risk management
- Optimizing resource allocation based on strategic positioning
The book includes:
- Detailed explanations of each gameplay type
- Real-world examples of successful gameplay implementation
- Frameworks for selecting and combining gameplays
- Strategies for adapting gameplays to different industries and contexts
-
Navigating Inertia: Understanding Resistance to Change in Organisations
- Author: Mark Craddock
- Part of the Wardley Mapping series (5 books)
- Available in Kindle Edition
- Amazon Link
This comprehensive guide explores organizational inertia and strategies to overcome it:
Key Features:
- In-depth exploration of inertia in organizational contexts
- Historical perspective on inertia's role in business evolution
- Practical strategies for overcoming resistance to change
- Integration of Wardley Mapping as a diagnostic tool
The book is structured into six parts:
- Understanding Inertia: Foundational concepts and historical context
- Causes and Effects of Inertia: Internal and external factors contributing to inertia
- Diagnosing Inertia: Tools and techniques, including Wardley Mapping
- Strategies to Overcome Inertia: Interventions for cultural, behavioral, structural, and process improvements
- Case Studies and Practical Applications: Real-world examples and implementation frameworks
- The Future of Inertia Management: Emerging trends and building adaptive capabilities
This book is invaluable for:
- Organizational leaders and managers
- Change management professionals
- Business strategists and consultants
- Researchers in organizational behavior and management
-
Wardley Mapping Climate: Decoding Business Evolution
- Author: Mark Craddock
- Part of the Wardley Mapping series (5 books)
- Available in Kindle Edition
- Amazon Link
This comprehensive guide explores climatic patterns in business landscapes:
Key Features:
- In-depth exploration of 31 climatic patterns across six domains: Components, Financial, Speed, Inertia, Competitors, and Prediction
- Real-world examples from industry leaders and disruptions
- Practical exercises and worksheets for applying concepts
- Strategies for navigating uncertainty and driving innovation
- Comprehensive glossary and additional resources
The book enables readers to:
- Anticipate market changes with greater accuracy
- Develop more resilient and adaptive strategies
- Identify emerging opportunities before competitors
- Navigate complexities of evolving business ecosystems
It covers topics from basic Wardley Mapping to advanced concepts like the Red Queen Effect and Jevon's Paradox, offering a complete toolkit for strategic foresight.
Perfect for:
- Business strategists and consultants
- C-suite executives and business leaders
- Entrepreneurs and startup founders
- Product managers and innovation teams
- Anyone interested in cutting-edge strategic thinking
Practical Resources
-
Wardley Mapping Cheat Sheets & Notebook
- Author: Mark Craddock
- 100 pages of Wardley Mapping design templates and cheat sheets
- Available in paperback format
- Amazon Link
This practical resource includes:
- Ready-to-use Wardley Mapping templates
- Quick reference guides for key Wardley Mapping concepts
- Space for notes and brainstorming
- Visual aids for understanding mapping principles
Ideal for:
- Practitioners looking to quickly apply Wardley Mapping techniques
- Workshop facilitators and educators
- Anyone wanting to practice and refine their mapping skills
Specialized Applications
-
UN Global Platform Handbook on Information Technology Strategy: Wardley Mapping The Sustainable Development Goals (SDGs)
- Author: Mark Craddock
- Explores the use of Wardley Mapping in the context of sustainable development
- Available for free with Kindle Unlimited or for purchase
- Amazon Link
This specialized guide:
- Applies Wardley Mapping to the UN's Sustainable Development Goals
- Provides strategies for technology-driven sustainable development
- Offers case studies of successful SDG implementations
- Includes practical frameworks for policy makers and development professionals
-
AIconomics: The Business Value of Artificial Intelligence
- Author: Mark Craddock
- Applies Wardley Mapping concepts to the field of artificial intelligence in business
- Amazon Link
This book explores:
- The impact of AI on business landscapes
- Strategies for integrating AI into business models
- Wardley Mapping techniques for AI implementation
- Future trends in AI and their potential business implications
Suitable for:
- Business leaders considering AI adoption
- AI strategists and consultants
- Technology managers and CIOs
- Researchers in AI and business strategy
These resources offer a range of perspectives and applications of Wardley Mapping, from foundational principles to specific use cases. Readers are encouraged to explore these works to enhance their understanding and application of Wardley Mapping techniques.
Note: Amazon links are subject to change. If a link doesn't work, try searching for the book title on Amazon directly.
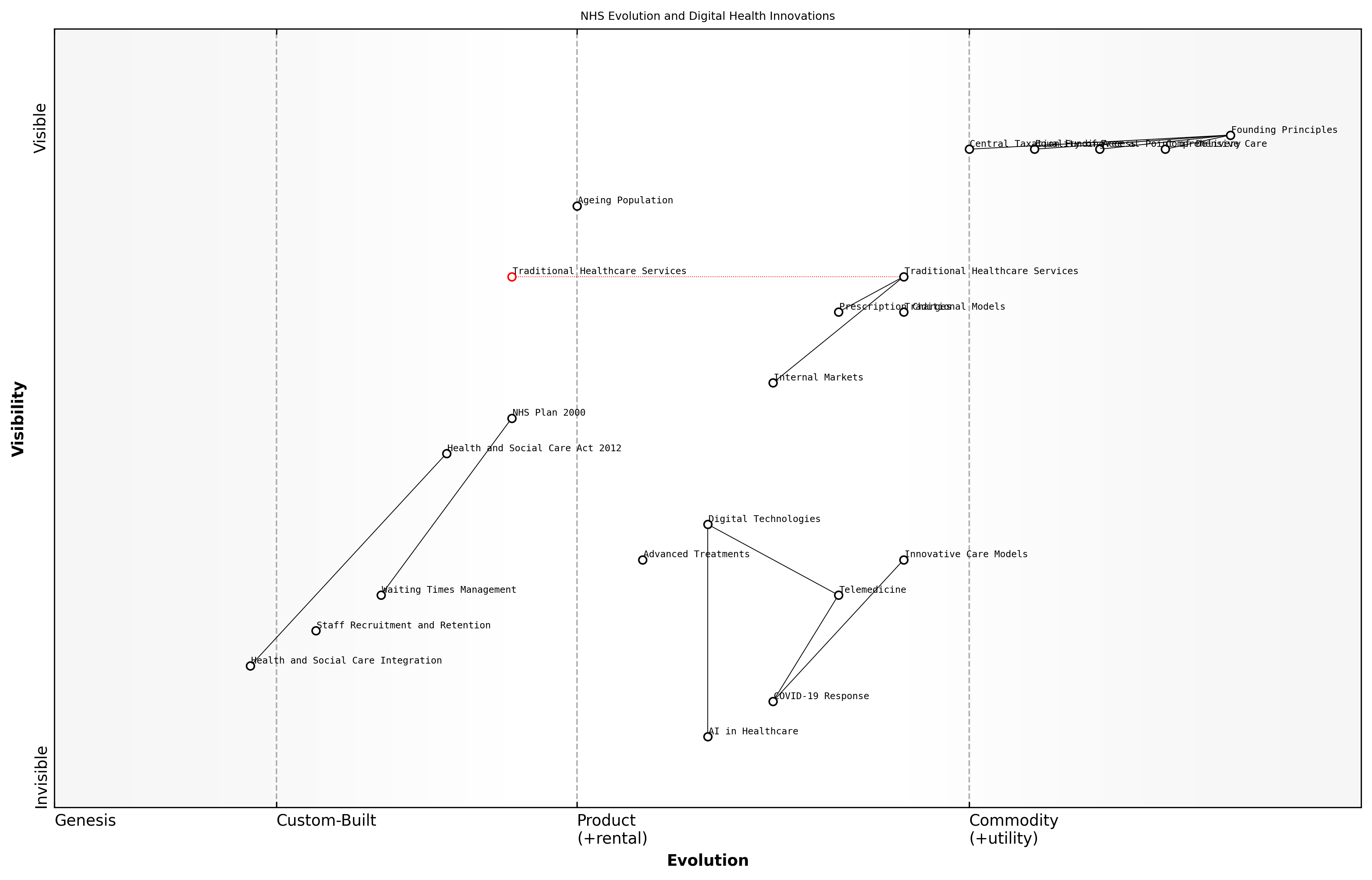
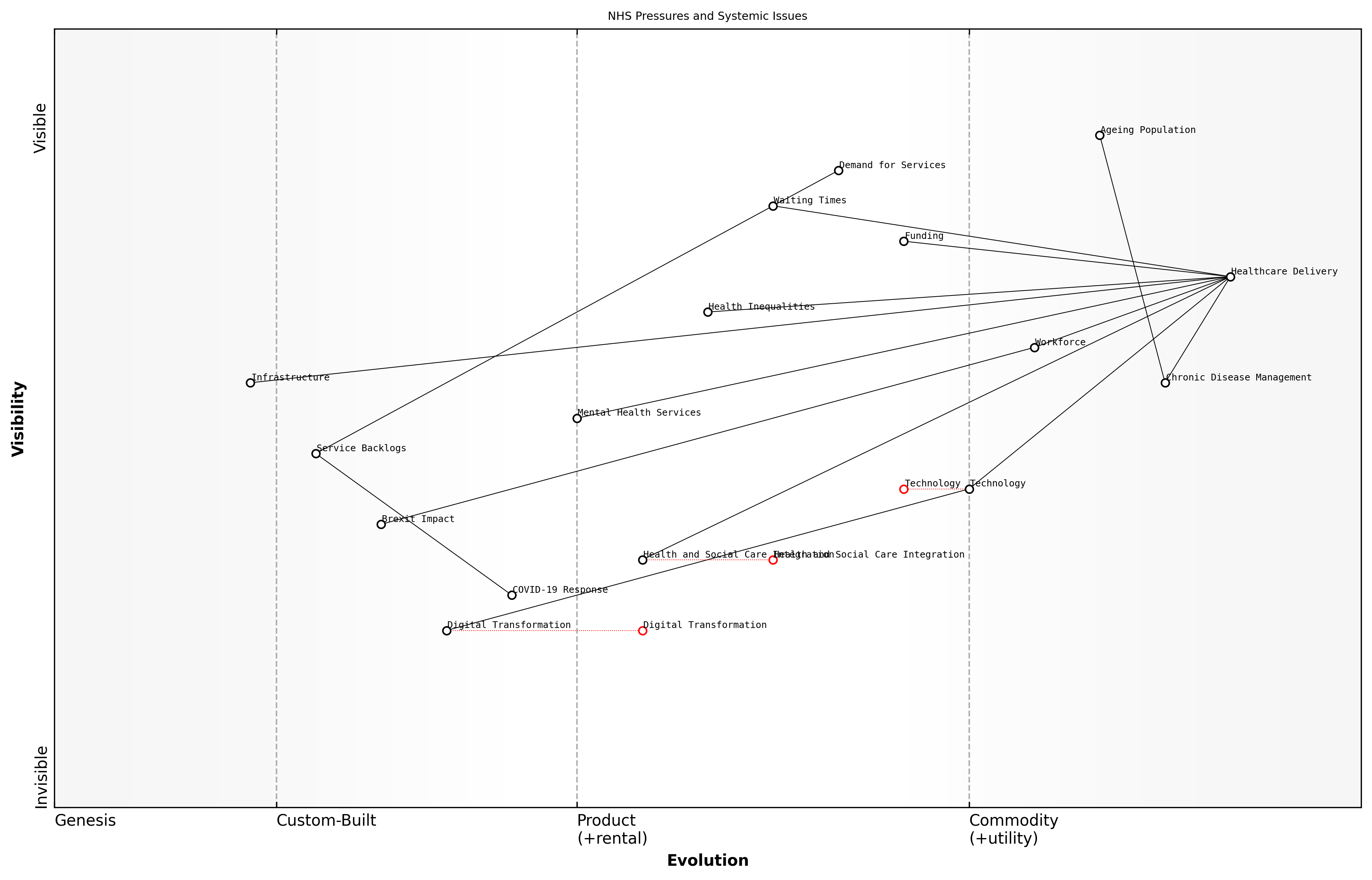
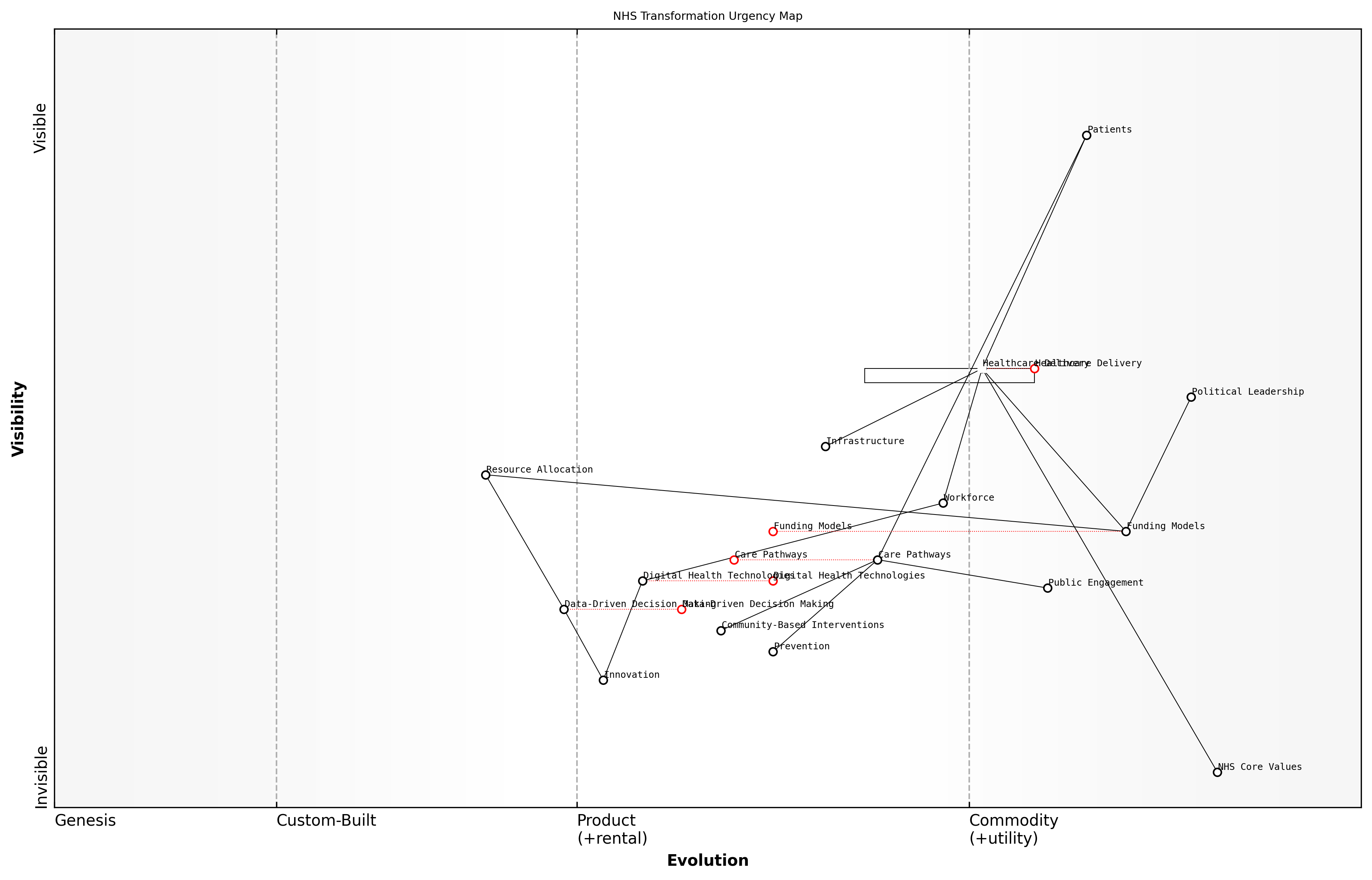
![Draft Wardley Map: [Insert Wardley Map illustrating the interconnections between key reform areas and their evolution stages]](https://images.wardleymaps.ai/map_2ca73409-ecbb-47fc-b87f-f10c051d0ec9.png)